No deposit Free Spins & Bonuses Southern Africa 2024
Content
The brand new betting requirements will be up to x20, meaning for many who earn $40 regarding the bonus, you will have to wager $800 in order to withdraw your payouts. A casino welcome added bonus are a marketing for brand new people in order to interest these to sign in within the an enthusiastic on-range gambling enterprise. (more…)
What to Expect During and After a Weight Loss Injection Treatment
Team Metabolic Health
At some point, many people can attest to attempting to lose weight. In fact, it’s estimated that 45 million Americans go on a diet each year in order to shed some stubborn pounds. While weight loss can be as simple as calories in versus calories out, everybody is unique and yields different results. What works for one person, doesn’t work out for the other, leading to feelings of hopelessness and inadequacy when weight loss goals aren’t being met. Fortunately, weight loss injections have taken the world by storm when it comes to achieving your dream body. What can you expect during and after a weight loss injection treatment? Are weight loss injections right for you? Read on to learn more. The Studio Med Spa offers a variety of weight loss injection treatments to help people attain the body they’ve been working for!
How Can I Obtain Weight Loss Injection Treatments?
Nowadays, lifestyle, age, and other factors can put a grinding halt to your weight loss. Weight loss injections are a safe treatment that allows people to be closer to their goals, without completely changing their lives. It should be noted that weight loss injections work even more effectively if a person is eating better and moving their body. If you are looking to obtain weight loss injection treatments, talk with an expert at The Studio Med Spa. Consultation for weight loss injection treatments includes looking at your individual weight loss goals, metabolism, medical history, diet, and more.
What Are My Options?
The most popular weight loss injections include:
Semaglutide which consists of GLP-1 receptor agonists. These agonists mimic the naturally developed hormone within the body known as GLP-1, to reduce appetite and regulate hunger cues for a lower calorie intake.
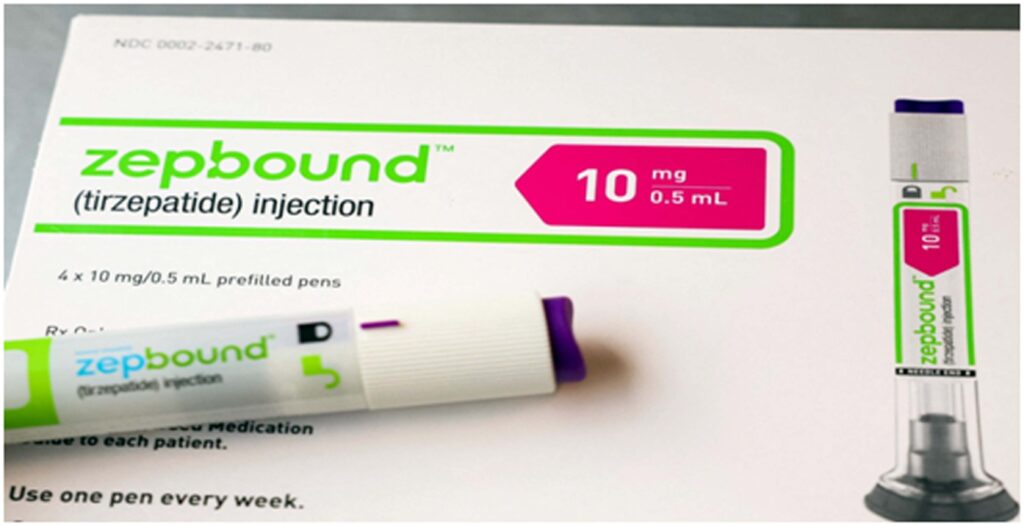
Tirzepatide is a much more potent weight loss injection compared to semaglutide. This injection treatment works as a dual receptor agonist for GLP-1 and GIP hormones in the body, helping to curb appetite and also slow down the digestion process and leave people feeling fuller longer.
What is the Process During the Injection?
The injection process for weight loss treatments is generally fast. Many people find the process takes anywhere from five to fifteen minutes. The injection is applied through a subcutaneous injection in an area of fatty tissue, most commonly the abdomen. Since the injections are not administered in the muscle, very fine needles are used, which also help to minimize feelings of pain and discomfort in patients. The best part is that these injections can be applied once a week, once every two weeks, or through a timeline that best fits your weight loss goals.
What Do I Have to Do After the Injection Treatment?
After the weight loss injection is administered, many people worry that they will have to take the day off from work. However, this is far from the case. Many people find themselves leaving the med spa clinic and jumping into their routine immediately. In fact, with an injection such as a Skinny Shot, a lot of individuals feel a burst of energy that allows them to tackle a massive to-do list they may not have wanted to do before! After the injection treatment is complete, all you have to do is let the injection run its course and go about your daily life.
Are There Any Side Effects?
Many people often ask if there are side effects from weight loss injection treatments. It is important to note that the side effects of these injections are typically very mild. The most common side effects include: Nausea, Fatigue, Dizziness, Stomach pain, Low blood sugar, Redness, tenderness, or pain in the injection site. These side effects do not take long to clear. The best part is there is no further maintenance needed for weight loss injections in the form of additional medication. One injection is all it takes to give you that much-needed boost to your weight loss goals!
Looking into Weight Loss Injections, But Unsure Where to Start?
Do you wonder if weight loss injections are right for you? Weight loss can be a long stubborn process for many. Many people often find themselves giving up when it takes longer to achieve their ideal body weight. Body injections have become a promising treatment that allows people to enhance their weight loss journey, without necessarily interrupting their busy routines. Weight loss injections have been deemed safe for administration, and many people can testify to how these injections have helped shed those last few pounds.
The process during and after the injection administration is relatively fast and easy, with minimal side effects recorded. Are you looking into weight loss injections? Unsure which treatment may be the right choice for you? Booking a consultation with a trustworthy and certified med spa clinic can help you learn about each treatment and which specific choice may align with your goals and needs. Call The Studio Med Spa to book your consultation now, and take the first step toward that goal body!
Credit: studiospa.com
Tirzepatide vs Semaglutide – What’s the Difference?
Team Metabolic Health
In the evolving world of weight loss advancements, two notable medications, Tirzepatide injections vs Semaglutide injections, have emerged as powerful tools in the fight against obesity and type 2 diabetes. Both drugs are praised for their efficacy in controlling appetite, reducing weight, and managing blood sugar levels, but they differ in composition and mechanism. This article delves into the distinct features, uses, and effects of each medication to help you understand what’s the difference between Semaglutide and Tirzepatide.

What Do Tirzepatide vs Semaglutide Share?
Tirzepatide vs Semaglutide are distinct in their mechanisms yet share crucial similarities that position them as powerful contributors in managing obesity, type 2 diabetes, and appetite control. Both drugs belong to the incretin modulator category, effectively targeting hormones that regulate metabolism, reduce appetite, and enhance insulin secretion. As synthetic peptides, Tirzepatide and Semaglutide boost the body’s natural insulin response, decrease appetite, and promote better blood glucose control and weight loss outcomes.
Tirzepatide vs Semaglutide: Scientific Comparison
Both Tirzepatide and Semaglutide fall under the category of incretin mimetics. Incretins are gut hormones released immediately after eating, significantly influencing insulin production by the pancreas. Both medications target GLP-1 (glucagon-like peptide-1) to enhance the body’s insulin response, lower blood sugar levels, and reduce appetite.
Key Mechanisms of Action
GLP-1 Activation: Both Tirzepatide and Semaglutide mimic GLP-1 activity to increase insulin secretion when blood sugar levels are elevated, regulate glucose absorption in the stomach, and decrease hunger signals. While both medications share GLP-1 activation, Tirzepatide also targets GIP (glucose-dependent insulinotropic polypeptide) receptors, enhancing its impact on insulin release and metabolic regulation.
Tirzepatide vs Semaglutide—Layman’s Explanation
Imagine GLP-1 as a “helpful signal,” guiding your body to process sugar slowly and feel satisfied after smaller meals. Both Tirzepatide and Semaglutide amplify this signal, helping your body focus on better blood sugar management and allowing you to feel fuller longer, reducing excessive calorie intake. Tirzepatide, however, offers an additional boost by acting on GIP receptors, further enhancing insulin response and promoting efficient weight reduction.
Tirzepatide vs Semaglutide—What’s the Difference?
The main difference between Tirzepatide vs Semaglutide lies in the dual receptor action of Tirzepatide. Unlike Semaglutide, which targets only GLP-1 receptors, Tirzepatide acts on both GLP-1 and GIP receptors. This dual mechanism results in a more pronounced effect on insulin sensitivity, blood sugar control, and weight loss. HydraMed client reporting have shown that Tirzepatide may provide superior weight loss results for some individuals due to its broader mechanism of action, making it a potentially more effective treatment for patients looking for significant health improvements.
Shared Benefits of Tirzepatide & Semaglutide
Both Tirzepatide & Semaglutide lead to similar health benefits, which include:
Weight Loss: By enhancing feelings of fullness and reducing appetite, both medications can significantly reduce body weight. Feedback has shown that individuals using these medications can experience considerable weight loss, making them powerful tools for managing obesity.
How They Work As A Peptide Primer
Both Tirzepatide injections and Semaglutide injections are part of a class of medications known as incretin mimetics. Here’s how they work:
Peptides as Master Keys: These medications are synthetic peptides that mimic natural hormones in the body. They act like master keys that unlock specific responses in the brain and digestive system to control appetite and insulin.
Biological Mechanisms: By activating GLP-1 receptors, these drugs increase insulin release in response to meals, slow down digestion, and signal fullness to the brain, reducing overall calorie intake.
Real-World Impact: This translates to less hunger, better control over eating, and improved blood sugar levels, which are crucial for weight management and diabetes control.
Comparing Mechanisms Between Tirzepatide vs Semaglutide
Peptides like Tirzepatide vs Semaglutide function as master keys that unlock specific bodily processes, particularly those involved in appetite regulation and glucose control. These medications mimic natural hormones that signal the brain to feel full and satisfied, effectively reducing calorie intake and promoting weight loss. While both Tirzepatide and Semaglutide activate GLP-1 receptors, Tirzepatide injections goes a step further by also stimulating GIP receptors. This dual action not only broadens its impact on glucose control but is also believed to significantly enhance weight loss outcomes compared to medications that target GLP-1 receptors alone. Both Tirzepatide and Semaglutide represent significant advances in the management of weight and metabolic health.
Tirzepatide vs Semaglutide for Weight Loss
Feedback indicates that Tirzepatide generally results in greater weight loss than Semaglutide, positioning it as a potentially more effective solution for individuals with severe obesity or those who have not achieved desired weight management results with other treatments. The enhanced weight loss observed with Tirzepatide can be attributed to its dual-receptor action, which not only improves glucose metabolism but also significantly impacts body weight regulation.
Tirzepatide vs Semaglutide in Controlling Hunger and Cravings
Both Tirzepatide vs Semaglutide effectively reduce hunger and appetite, pivotal factors in successful weight management. However, Tirzepatide appears to have a slight advantage in decreasing calorie intake. This edge is likely due to its ability to act on both GLP-1 and GIP receptors, enhancing the feeling of fullness and satisfaction after meals and leading to a more substantial reduction in overall calorie consumption.
Administration: Injections and Shots
Both Tirzepatide and Semaglutide are administered through injections, typically once a week. This method ensures the medication is delivered efficiently and maintains consistent levels in the bloodstream.
Tirzepatide vs Semaglutide Side Effects
The common side effects associated with both Tirzepatide and Semaglutide are primarily gastrointestinal in nature, including nausea, vomiting, diarrhea, and constipation. These side effects are typically manageable and often decrease over time as the body adjusts to the medication. However, both medications can occasionally lead to more serious side effects, such as pancreatitis and renal impairment. These severe side effects are rare but require immediate medical attention should they occur, underscoring the importance of close monitoring by healthcare professionals during treatment.
Side Effects of Tirzepatide
Like all medications, Tirzepatide can have side effects, which typically include gastrointestinal issues such as nausea, vomiting, and diarrhea. These are generally mild and decrease over time.
Side Effects of Semaglutide
Semaglutide also shares similar side effects, with gastrointestinal distress being the most common. Patients may experience nausea, constipation, or mild abdominal pain.
How to Choose the Right Option for You
Choosing between Tirzepatide and Semaglutide can feel overwhelming, but it really comes down to understanding your own health needs and goals. Here are a few steps to help guide you in making the best decision:
Consult Your Healthcare Provider: Always start with professional medical advice. Discuss your overall health, medical history, and any specific conditions like diabetes that might affect your choice.
Consider Your Weight Loss Goals: Are you looking for significant weight reduction, or is your focus more on controlling blood sugar levels? While both medications help with weight loss, Tirzepatide’s dual-action may offer an edge if your primary goal is more substantial weight loss.
Evaluate Side Effects: Both drugs have similar side effects, but individual tolerances can vary. Consider how you handle gastrointestinal discomfort or other potential side effects.
Assess Lifestyle Fit: Think about how each treatment fits into your lifestyle. This includes considering the weekly injection schedule and any other medication routines you already have.
Budget Considerations: Review the cost of each medication with your insurance provider to understand the financial impact of your choice.
Credit: hydramed.com/blog
Manual Testing vs Automation Testing
In general, automated end-to-end tests are expensive, slow, and inconsistent unless well-maintained and well-written. With the traditional Waterfall model, QA testing happened late in the software development life cycle (SDLC). The QA team would provide feedback to the development team at the end of a given development cycle, and the development team would then fix as many bugs as they could. Usability is all about creating highly interactive and engaging user experiences. That is why QA professionals use manual testing to check software functionalities and various scenarios in user behavior. Hardly can automated testing ensure what color type, images, or fonts are appropriate for creating eye-catching user interfaces.
Tests where you must explore features and app behavior, such as Usability Testing, Exploratory Testing, and Manual Testing, should be prioritized. Whereas for Regression Testing and for those tests where scalability and test coverage is the priority, Automation Testing should be prioritized. Teams perform several types of system testing, manual qa courses like regression testing, stress testing, functional testing, and more, depending on their access to time and resources. As you can see, there are numerous reasons why you should acquire automated testing skills. In addition to above-average job growth, you can anticipate strong earnings potential as a QA automation engineer.
Best Practices for QA Testing
Anyone who’s been in the QA field for awhile (or Engineering in general!) is familiar with the Agile QA process in software development. Test automation eases the burden of managing the various parts of the testing process. It enables the QA team to use their time to create effective test cases.
Automated testing can bring several advantages to the QA process and indeed, to the SDLC. Additionally, automated tests bring advantages to a codebase that manual QA testing cannot, such as code confidence and maintainability. Manual testing, including exploratory testing and usability testing, is vital in the software development life cycle. And development teams would do well to keep this golden rule in mind. To create stable software, teams should look to both manual testing and automated testing and make each one a core part of their SDLC. There are many pros and cons to automated testing, but ultimately creating stable software necessitates both automated and manual quality assurance testing.
Manual Testing vs. Automated Testing
Despite a continuous buzz around the automated testing, manual one is still important. Particularly, mobile devices and wearables do require manual testing to check what bottlenecks they might have in our daily lives. A key to getting all the automation testing benefits is to blend it successfully with manual testing.

Ozempic can even cut the risk of Alzheimer’s disease, study says
Team Metabolic Health
A new study found that semaglutide, the active ingredient in Ozempic and Wegovy, lowered the risk of Alzheimer’s disease in people with type 2 diabetes
Novo Nordisk’s blockbuster drug Ozempic (NVO-0.35%) is linked to yet another health benefit. This time it’s lowering the risk of Alzheimer’s disease.
People who are prescribed semaglutide — the active ingredient in Ozempic and Wegovy — as a treatment for type 2 diabetes may have a reduced risk of Alzheimer’s disease, according to a new study published Thursday in the scientific journal Alzheimer’s & Dementia.
The study found that prescriptions for semaglutide were associated with a lower risk of an Alzheimer’s diagnosis compared to people taking other diabetes medications, including other GLP-1 drugs.

Ozempic is medicine for adults with type 2 diabetes that along with diet and exercise may improve blood sugar. While some doctors are prescribing it “off label” for weight loss. Image: Steve Christo – Corbis/Contributor (Getty Images)
Semaglutide is part of the GLP-1 class of medications, which mimic a hormone that regulates appetite and blood sugar. These medications have become highly sought after for their remarkable effectiveness in treating obesity and type 2 diabetes. Other GLP-1 treatments include Eli Lilly’s (LLY+4.38%) Mounjaro and Zepbound.
Researchers in this study analyzed the electronic records of more than 1 million patients with type 2 diabetes who had no previous diagnosis of Alzheimer’s disease over a three-year period.
The study found that semaglutide was associated with a 40% to 70% reduced risk of a first-time Alzheimer’s disease diagnosis compared to patients taking other diabetes medications.
The study authors noted that semaglutide has been shown to address several factors linked to Alzheimer’s, including weight, heart health, alcohol use, smoking, and depression. They suggested that, due to its impact on these risk factors, semaglutide may help reduce the risk of developing Alzheimer’s disease in high-risk patients.
The researchers also added that their findings support the need for further clinical trials to evaluate semaglutide’s potential in delaying or preventing Alzheimer’s disease.
As of 2024, an estimated 6.9 million Americans aged 65 and older live with Alzheimer’s disease, a figure expected to nearly double to 13.8 million by 2060.
Credit: Quartz
Weight loss drugs could help with alcohol and opioid addiction, new study shows
Team Metabolic Health
Diabetes and weight loss drugs like Mounjaro and Ozempic may also help patients suffering from addiction, according to a new study.
In the study, published in the scientific journal Addiction, researchers found people with opioid or alcohol use disorder who take Ozempic or similar medications appear to have a 40% lower rate of opioid overdose and a 50% lower rate of alcohol intoxication compared to people who aren’t on the medications.
Dr. Céline Gounder, CBS News medical contributor and editor-at-large for public health at KFF Health News, said these are “significant clinical impacts for patients.”
The study used a large data set, looking at almost 10 years of data from patients in over 100 health systems across the country.
Previous research has also looked at whether the medications may help people quit smoking.
Gounder says it’s possible we’ll see these drugs prescribed primarily for addiction treatment in the future, but more study is needed.
“We would need to see some randomized clinical trials over time to prove that this is truly cause and effect. That’s what you would need also for the FDA to expand the indication, which paves the way also for insurance coverage. But I think it’s quite possible we see that down the line,” she said on “CBS Mornings.”
That doesn’t mean these drugs don’t have risks, though, Gounder cautioned.
“These drugs are working on the brain, and we don’t know what the long term effects of having this kind of hormone impacting your brain would be. We don’t know what the risks in the long term for cancer would be,” she said. “We know that there are risks of pancreatitis, gallbladder issues, kidney issues, and there are some reports of suicidal thoughts, so that would be a concern.”
Credit: cbsnews.com
Play Miracle Tree Position On the internet free of charge Demo, Opinion
There is also an enthusiastic expiration go out to your extra bucks, definition you’ll must complete the betting standards inside the stated go out physique. You’re going to get your own totally free spins as soon as you complete the subscription process and certainly will provides one week to do the newest betting element 10x for the slots and you will 20x on the any online game. (more…)
10 reasons why you are gaining weight despite exercise and healthy diet: Nutritionist lists common mistakes to avoid
Team Metabolic Health
So, you hit the gym or work out from home and eat healthy, but still gain a couple of kilos overnight? If that’s the case, here’s what you need to know.
Are you trying to lose weight fast? You may be aware that your diet and workout routine and making small changes to your lifestyle can help you see results. Certified fitness and nutrition coach Shitija, in a recent Instagram post, highlighted how you can follow a healthy diet and consistently work out, but still gain weight.

How do you know you’re losing body fat if the scale doesn’t show it? Find out. (Unsplash)
She wrote, “You need to share this with someone who is too scared of weighing scale and needs to know this! Women can eat healthy, exercise, and still see a 2-pound (almost 1 kg) increase overnight. Does this happen to you? It’s frustrating, especially when you keep hearing everywhere the ‘calories in versus calories out’ kind of advice. Let me tell you that’s not the whole truth.”
Reasons you are putting on weight
Shitija then listed 10 common causes for the weight gain:
1. High-carb dinner
2. Stress
3. Heavy workout
4. Late dinner
5. Menstrual cycle
6. Poor sleep
7. Need to poop
8. Sodium-rich meal
9. Feeling unwell
10. Weighing at a different time
Shitija also said, “Remember, most of these are due to water retention or inflammation, and not fat. You didn’t eat 7000 calories by accident! But how do you know you’re losing body fat if the scale doesn’t show it?”
Shitija added, “Use these tips to track real progress, not just the number on the scale. Stay calm and remember, weight fluctuations are normal!”
Disclaimer: This article is for informational purposes only and not a substitute for professional medical advice. Always seek the advice of your doctor with any questions about a medical condition.
Credit: Hindustan Times
Lilly to offer single-dose vials of weight-loss drug on telehealth platform Ro
Team Metabolic Health
An injection pen of Zepbound, Eli Lilly’s weight loss drug, is displayed in New York City, U.S., December 11, 2023. REUTERS/Brendan McDermid/File Photo
Dec 11 (Reuters) – Telehealth company Ro said on Wednesday it will offer single-dose vials of Eli Lilly’s (LLY.N), weight-loss drug Zepbound to patients with obesity, becoming the first alternative platform for the lower-cost version of the drug to Lilly’s own website.
In August, Lilly started selling vials of the lowest starter dose of Zepbound in the U.S. through its direct-to-consumer website LillyDirect.
“Offering Zepbound single-dose vials … through another platform to LillyDirect will help ensure broader availability,” said Patrik Jonsson, president of Lilly Cardiometabolic Health.
The 2.5 milligram and 5 mg vials, the lowest doses of the drug cost $399 and $549, respectively, for a month’s supply on Lilly’s website. The vials are available for the same price through Ro, the telehealth firm said.
Ro said it is directly integrated with LillyDirect’s self-pay pharmacy. “No one else is currently working with Lilly on that, we’re the first,” a Ro spokesperson added.
The telehealth firm also helps fill prescriptions for Novo Nordisk’s (NOVOb.CO), rival weight-loss drug Wegovy.
Besides branded medicine, Ro also offers a copycat version of Novo’s medicine that can be made and supplied by compounding pharmacies as long as the branded drug is in shortage.
Ro said it also used to offer a compounded version of the Lilly drug, but does not currently offer it.
Shortages of weight-loss drugs have pushed patients to cheaper compounded versions, which can be sold and distributed in bulk as long as the original drug is on the U.S. Food and Drug Administration’s shortage list.
Lilly and Novo have been looking to get the drugs off the shortage list to curtail the market for online pharmacies.
In early October, the FDA removed Zepbound and Mounjaro from its shortage list. However, in the face of a lawsuit brought by compounders, the FDA decided they can continue to make copies while the agency reevaluates whether there is sufficient supply.
Credit: Reuters
Why ‘digital twins’ could speed up drug discovery
Team Metabolic Health
This is the first of a six-part series on how AI is changing medical research and treatments.
The heart in front of me beats and moves like a human organ, but has no blood flowing through it, nor does it live in a human body.
It’s a computer-generated heart, or digital twin, used to test implantable cardiovascular devices, like stents, and prosthetic valves that, once confirmed they are safe, will eventually be used on real people.
But the heart’s creators, Adsilico, have gone beyond just creating one accurate model.
Using artificial intelligence and huge amounts of data, they have created multiple different hearts.

This is the first of a six-part series on how AI is changing medical research and treatments.
The heart in front of me beats and moves like a human organ, but has no blood flowing through it, nor does it live in a human body.
It’s a computer-generated heart, or digital twin, used to test implantable cardiovascular devices, like stents, and prosthetic valves that, once confirmed they are safe, will eventually be used on real people.
But the heart’s creators, Adsilico, have gone beyond just creating one accurate model.
Using artificial intelligence and huge amounts of data, they have created multiple different hearts.
These AI-generated synthetic hearts can be made to reflect not just biological attributes like weight, age, gender and blood pressure, but health conditions and ethnic backgrounds.
As these differences often aren’t represented in clinical data, digital twin hearts can help device manufacturers conduct trials across more diverse populations than they could with human trials, or trials involving just digital twins without AI.
“This allows us to capture the full diversity of patient anatomies and physiological responses, which is not possible using conventional methods. This use of AI to enhance device testing leads to the development of devices that are more inclusive and safer,” says Adsilico chief executive Sheena Macpherson.
In 2018 an investigation by the International Consortium of Investigative Journalists revealed that 83,000 deaths and over 1.7 million injuries were caused by medical devices.
Ms Macpherson hopes that AI powered digital twins can cut down those numbers.
“To really make these devices safer, you need to test them more thoroughly, and it isn’t feasible to do that in a clinical trial environment due to the expense of it,” says Ms Macpherson, who is based in Northumberland.
“So you want to be able to use the computer-generated version, to make sure that whatever you’re doing, you’ve tested it as thoroughly as possible before you test it on a human.
“Even a fraction of those deaths – and the associated lawsuits – could have been avoided with more thorough testing. You can also get more detailed results.
“You could take the same [virtual] heart and you could test under low or high blood pressure, or against different disease progression, to see whether that affects the device in any way.”
Ms Macpherson adds: “[Virtual] testing gives medical device manufacturers many more insights. It also means that we can test in other sub patient groups, not just white men which clinical trials have traditionally been based on.”
Adsilico’s AI models are trained on a combination of cardiovascular data, and data from real MRI and CT scans, that includes medical imaging from consenting patients.
The data draws from detailed anatomical structures of the heart, to help create accurate digital representations of how medical devices will interact with different patient anatomies.
Adsilico’s trials involve the creation of a digital twin of the device to be tested, which is then inserted into the virtual heart in an AI-generated simulation.
It all takes place inside a computer, where the test can be replicated across thousands of other hearts – all AI-simulated versions of a real human heart. Human and animal trials, on the other hand, tend to involve just hundreds of participants.
Perhaps the biggest incentive for drug and device manufacturers to supplement clinical trials with AI digital twins is how it reduces the time it takes, which translates into big cost savings, too.
Drug manufacturer Sanofi, for example, hopes to reduce the testing period by 20%, while also increasing the success rate. It is using digital twin technology in its immunology, oncology and rare disease specialism.
Using biological data from real people, Sanofi creates AI-based simulated patients – not actual clones of specific individuals – that can be interspersed across the control and placebo groups within the trial.
Sanofi’s AI programmes also then creates computer-generated models of the drug to be tested, synthesising properties like how the drug would be absorbed across the body, so it can be tested on the AI patients. The programme predicts their reactions, too – replicating the real trial process.
“With a 90% failure rate across the industry of new drugs during clinical development, an increase of just 10% in our success rate by using technologies like digital twins could result in $100m in savings, given the high cost of running late phase clinical trials,” says Matt Truppo, Sanofi’s global head of research platforms and computational research and development.
The results so far have been promising, Mr Truppo, who is based in Boston, US, adds.
“There is still a lot to do. Many of the diseases we are now trying to impact are highly complex. This is where tools like AI come in. Powering the next generation of digital twins with accurate AI models of complex human biology is the next frontier.”
Digital twins might have weaknesses though, says Charlie Paterson, an associate partner at PA Consulting and a former NHS service manager.
He points out that the twins are only as good as the data that they are trained on.
“[Due to] aged data collection methods, and low representation of marginalised populations, we could end up in a position where we could still be introducing some of those biases when we’re programming virtual recreations of individuals.”
Working with limited legacy data to train its AI is an issue Sanofi is aware of and working to resolve.
To fill gaps in its internal data sets – made up of millions of data points from the thousands of patients that undergo its trials each year – it sources data from third parties, like electronic health records and biobanks.
Back at Adsilico, Ms Macpherson is hopeful that one day AI digital twin technology will eliminate animal testing from clinical trials, which is still currently considered an essential part of the drug and device testing process.
“A virtual model of our hearts is still closer to a human heart than that of a dog, cow, sheep, or pig, which tends to be what they use for implantable device studies,” she says.
Credit: BBC
Indian drugmakers are preparing for the launch of copycat weight-loss drugs as the world moves towards the patent expiry of Novo Nordisk’s blockbuster brands Ozempic and Wegovy
Team Metabolic Health
Indian drugmakers are preparing for the launch of copycat weight-loss drugs as the world moves towards the patent expiry of Novo Nordisk’s blockbuster brands Ozempic and Wegovy.
The Danish firm’s patents for semaglutide, the active pharmaceutical ingredient in its star brands, will start expiring in Asia (including India) and Africa in 2026 and in the US in 2030. While all eyes are on the Indian industry – known for its ability to produce generic drugs at a fraction of the cost – to cater to the soaring yet unmet demand for anti-obesity and anti-diabetic drugs, driving sales through price war won’t be easy this time.
Globally the demand for weight-loss drugs, specifically the glucagon-like peptide-1 (GLP-1) class of medications is “exploding”, experts told News18. The drug is used to treat type 2 diabetes and obesity and it works by mimicking the effects of the body’s natural hormone, GLP-1, which helps to reduce appetite, slow digestion, boost insulin production, and decrease the amount of sugar produced by the liver.
Health experts eagerly anticipate the launch of these drugs in India to meet the rising demand. It’s important to remember that India is known as the “diabetes capital of the world”, and the latest Economic Survey report reveals that the rate of adult obesity in the country has more than tripled.

It’s important to remember that India is known as the ‘diabetes capital of the world’, and the latest Economic Survey report reveals that the rate of adult obesity in the country has more than tripled. Representational Image
Popular endocrinologist Dr Anoop Misra told News18 that semaglutide and other advanced drugs in this class are “impactful, offering a range of significant health benefits”.
“Their use is expected to rise sharply,” said Misra, who is chairman of Fortis C-Doc Hospital for Diabetes and Allied Sciences. “However, cost remains a significant concern, and the availability of affordable alternatives, such as generics for Ozempic, is crucial for India where obesity and diabetes are on the rise.”
As research progresses, Misra said, “We anticipate even more potent medications on the horizon that could offer substantial benefits for individuals with severe obesity.”
Misra’s expectations align with the industry’s strategy—to introduce improved medicines that are more effective than current options like Ozempic but at a significantly lower cost.
Will loss of patent bring prices down?
The Indian market for GLP-1 drugs is yet to open up fully due to the unavailability of these top brands, with affordability also being a significant barrier. It means that while Ozempic or many other top-selling versions are not in India and even if they were, they could have been unaffordable for many Indians.
According to Novo Nordisk’s website, the price of an Ozempic pen (0.25 or 0.5 mg) is $968.52, which translates to over Rs 81,000. But, the local drug dealers claim to import and sell the injection for Rs 20,000 per shot.
However, the market for this category may not move as it does for other generic drugs where the price of generic drugs falls dramatically. In fact, experts cautioned that moving further, the price of the copycat version of the majority of GLP-1 class drugs or semaglutide may not crash heavily. The reason is that these drugs follow a complex manufacturing process very similar to making biological products.
To put it in perspective, semaglutide is a polypeptide and was originally classified as a biologic. However, under the FDA’s newly revised definition, it is no longer classified as a biologic because it contains fewer than 40 amino acids.
Vishal Manchanda, pharma analyst at financial services firm Systematix, told News18 that the category registered annual sales of $50 billion this year which is almost twice the size of the Indian pharmaceutical industry.
“Generally, we expect prices to crash in the range of 80 to 90% after the drug loses its patent, but in this case, we must also consider that making this class of drugs is complex. Therefore, it remains to be seen whether the desired price reduction can be achieved or not.”
Currently, two innovators are dominating the $50 billion market : Novo Nordisk’s Ozempic or Wegovy (Semaglutide) and Eli Lilly’s Mounjaro/Zepbound (Tirzepatide).
Novo Nordisk had said that it has tripled Wegovy production over the last three years and will continue to ramp up at the same pace, but still, it is unable to serve the demand. “We still have a situation where there are far more patients who would like to have the treatment than what both Eli Lilly and we can supply,” CEO Lars Fruergaard Jorgensen told Reuters. This shows the huge demand and gap in supply.
Manchanda believes that in the coming two to three years, multiple other innovator brands will emerge in the global market with eight to ten brands coming from large credible players. “This is when the economics is going to change as the demand shortages will be plugged. People in developed markets will get even better options than existing ones and developing markets like India (which are being ignored by innovators) will gain attention.”
In short, it’s expected that the upcoming drugs are likely to have a better profile in terms of quicker weight loss and convenient dosage (such as oral pills instead of injections).
“Hence, in a few years from now, emerging markets (including India) will have multiple GLP-1 options to choose from,” Manchanda predicts. “Also, semaglutide generics will become available…While the price of semaglutide is expected to fall once generics are launched, it remains to be seen whether the reduction will be significant enough to greatly expand access or not.”
Indian pharma developing semaglutide, other GLP-1 drugs
Wegovy and Ozempic drove Novo Nordisk to record bumper sales since the launch. In fact, the success story has turned the Danish drugmaker into Europe’s most valuable firm. Estimates peg that the company’s market value of about $570 billion is more than its home country, Denmark’s, annual GDP.
While Novo Nordisk declines to comment on its plan to launch Ozempic or Wegovy in India (in an email sent by News18), it’s obvious that all major Indian generic manufacturers are closely monitoring the upcoming expiry of Novo Nordisk’s exclusivity on GLP-1 drugs.
Manchanda said that in India, at least five to six players are working on developing the generic versions including Sun Pharma, Biocon (which already has large-scale peptide drug-making experience), Dr Reddy’s, Zydus, Natco, Shilpa Medicare, and Aurobindo Pharma.
Furthermore, Novo Nordisk may also not step back once the drug’s patent expires. The company may lower its price and continue to compete in the market. “Majority of Indian firms have capabilities to manufacture peptides and they can certainly manufacture this complex category. But we also expect the innovator Novo Nordisk to compete with generic players and chase a majority share,” Manchanda added.
Dr Reddy’s Laboratories announced in an investor call that the company aims to have about “15 GLP-1 drugs” to treat obesity and diabetes, in its portfolio with various timelines.
In October, last year, the company received the nod for conducting a bioequivalence study for Ozempic (semaglutide injection) from the Drugs Controller General of India (DCGI) after it sought a waiver of the phase-III clinical trial of the drug and its market authorisation. It aims to bring in the generic version as soon as the patent expires.
A company spokesperson told News18 that while the product is under patent right now, Dr Reddy’s Labs “will definitely participate in the opportunity but we will be part of the generics entry when the patent expires”.
Bengaluru-based Biocon – which is known for its expertise in developing complex biosimilars – has become the first company to win UK authorisation to offer a generic version of Novo Nordisk’s other popular GLP-1 category drug liraglutide sold under the brand name Saxenda. The firm told the Financial Times that it is ready to launch sales by November.
In an interview with the Financial Times, Siddharth Mittal, chief executive officer, Biocon Limited, predicted, “When the generics come in there will be a huge price war…There is a huge demand for these drugs at the right price.”
Biocon’s spokesperson did not respond to News18’s request for comment seeking more information on its plans to launch anti-obesity drugs in India.
What’s cooking in Indian drugmakers’ research labs?
India’s top drugmaker, Sun Pharma, is working on developing the GLP-1 category drug Utreglutide. In June, it announced the results from the study showing significant weight loss, glucose-metabolic and lipid-lowering efficacy.
Another Mumbai-based drugmaker, Cipla, is also preparing to launch GLP-1 drugs in India, the US, and other emerging markets.
“GLP-1 for diabetes and obesity is a very big transformation, equivalent to statins for cholesterol control,” Umang Vohra, the company’s global CEO, said in a press briefing in January this year. “And I would like to believe there are 100 million diabetics (patients) in this country (India) and there are several that are not diagnosed. And I think if we were to even cover 20 or 25% of that population by using GLP-1, it’s going to be a very significant opportunity.”
He said that “Cipla will be looking (at hopping on the opportunity) for India, emerging markets, and the US [for semaglutide]. We may not be the first wave launcher in the US, but we have plans.”
Natco and Mylan have also collaborated on the development of generic Ozempic products.
Not only top pharma companies are keen to manufacture but the central government is also gearing up to make GLP-1 drugs under the flagship production-linked incentive (PLI) scheme.
Arunish Chawla, secretary, department of pharmaceuticals (DoP), told reporters in June that “the local pharmaceutical industry is already working on producing these drugs here after the patents expire around 2026″.
Without divulging details of which companies are working on it (citing competition sensitivity), he said: “Work has already begun on the same and soon GLP-1RA drugs will be made in India under the PLI scheme.”
While increased competition is certainly good news for patients, the real winner will likely be the company that offers the lowest cost and can meet the market’s demands on a large scale.
Credit: News18
MUSC involved in study on device that caused ‘statistically significant weight loss’
Team Metabolic Health
A device called Epitomee caused “statistically significant weight loss” in a 24-week trial involving nine study sites, including the Medical University of South Carolina. Patrick O’Neil, Ph.D., led MUSC’s involvement in the study. He described how the device works.
“It’s a capsule that you swallow, and it changes shape. The outer part of the capsule dissolves very quickly, as soon as it gets in the stomach. The inside of the capsule is this very absorbent polymer with some bonding materials. This can absorb about 100 times its weight in water from the stomach. So that causes the device to expand into a rigid triangular shape. And it stays in the stomach like that for a while,” O’Neil said.
The device gives a feeling of fullness. “It occupies space and mechanically stimulates receptors in the stomach during the few hours that it’s there. And so that can produce some stimuli that are associated with eating more food than you will have eaten,” O’Neil said.
It dissolves in about six hours and passes out of the body through the digestive system.
The study had about 280 participants across its nine locations. They took a capsule with two cups of water a half hour before a meal, two times a day. Half got Epitomee; half got a placebo capsule.

More than 70% percent of adults 20 and older are overweight, according to the Centers for Disease Control and Prevention. Photo Illustration Courtesy of UConn Center for Food Policy and Health
They all used an app to log every time they took a capsule, along with what they ate and drank. They also had activity monitors and smart scales that were connected to the app. And everyone got what O’Neil called state-of-the-art behavioral, dietary and exercise lifestyle coaching for weight loss by registered dietitians, using the data the participant uploaded to the app.
All participants were overweight at the start, with a body mass index ranging from 27 to 40. An average healthy body mass index is anywhere from 18.5 to less than 25, according to the Centers for Disease Control and Prevention. They could be prediabetic but not diabetic.
O’Neil, a professor in the Department of Psychiatry and Behavioral Sciences at MUSC, director of MUSC’s Weight Management Center and a former president of the Obesity Society, was pleased with the results. The average loss in the Epitomee group was 6.6% of start weight, compared with 4.6% in the placebo group, with substantial variability within each group. Fifty-six percent of the people in the Epitomee group lost at least 5% of their body weight in six months compared with 44% of the people in the placebo group. Some participants lost more than 15% of their body weight.
“If you look at it in comparison to what we see with semaglutide and tirzepatide these days, of course, it’s nowhere near that. But it’s not meant to compete with that. This is meant to fill a different need,” O’Neil said. Semaglutide is the key ingredient in some of the prescription diabetes and weight loss drugs that have come out in recent years, including Ozempic and Wegovy. Tirzepatide is in Mounjaro and Zepbound.
Unlike those products, O’Neil said the Epitomee capsule isn’t considered a medication but a device. The company that makes it, Epitomee Medical Ltd., calls it drug-free and easy to use. It announced Food and Drug Administration clearance of the device in September.
O’Neil was part of a team that presented the Epitomee study results at the Obesity Week 2024 conference in Texas this week, an event focused on science and treatment. He said he has no stake in the company. “They funded our site research site as they did all the other sites.”
O’Neil said the study found no serious adverse side effects in people who took Epitomee. It’s expected to become available in the U.S. next fall. It’s unclear what it will cost.
Credit: web.musc.edu
Analysis and study of perceptron to solve XOR problem IEEE Conference Publication
This aspect is critical as it directly affects the responsiveness and efficiency of NN applications. The XOR (Exclusive OR) logic gate operates on two double inputs, creating a genuine yield in case the inputs are diverse and an untrue yield in case they are the same. Three perceptrons will help to draw two straight lines, and the third one will intercept the region between these two lines. We have considered weights as -1, 1.2, and 1.2 as mentioned in the below truth table of OR gate. No, we can’t draw a line to separate two classes with MP neurons as the slope will be -1.
In the XOR problem, two-dimensional (2-D) data points are classified based on the region of their x- and y-coordinates using a mapping function that resembles the XOR function. If the x- and y-coordinates are both in region 0 or 1, then the data are classified into class “0”. In this problem, a single linear decision boundary cannot solve the classification problem. Instead, nonlinear decision boundaries are required to classify the data. These networks connect the inputs of artificial neurons to the outputs of other artificial neurons. We can separate two classes for all these types of input mentioned below.
This concept is fundamental to understanding the limitations of single-layer perceptrons, which can only model linearly separable functions. Of course, there are some other methods of finding the minimum of functions with the input vector of variables, but for the training of neural networks gradient methods work very well. They allow finding the https://traderoom.info/neural-network-for-xor/ minimum of error (or cost) function with a large number of weights and biases in a reasonable number of iterations. A drawback of the gradient descent method is the need to calculate partial derivatives for each of the input values. Very often when training neural networks, we can get to the local minimum of the function without finding an adjacent minimum with the best values. Also, gradient descent can be very slow and makes too many iterations if we are close to the local minimum.
The XOR problem is a classic example in the study of neural networks, illustrating the limitations of simple linear models. To solve the XOR problem, a neural network must be capable of learning non-linear decision boundaries. This requires a multi-layer architecture, typically involving at least one hidden layer.
- In training neural networks, particularly for the XOR problem, the selection of negative data is crucial.
- This problem is significant because it highlights the limitations of single-layer perceptrons.
- The XOR problem is a classic problem in artificial intelligence and machine learning.
- The output is then compared to the target value, and the error is calculated.
- If two classes of points can be perfectly separated by such a line or hyperplane, they are considered linearly separable.
- Let’s look at a simple example of using gradient descent to solve an equation with a quadratic function.
The network classifies the data into the “Blue” and “Yellow” classes. Implementing XOR neural networks presents unique challenges that require careful consideration and innovative solutions. Below are some of the primary challenges and strategies to address them. Come on, if XOR creates so much problems, maybe we shouldn’t use it as ‘hello world’ of neural networks? If I’ll try to add just 1 more neuron in the hidden layer, network is successfully calculating XOR after ~ epochs. A not-for-profit organization, IEEE is the world’s largest technical professional organization dedicated to advancing technology for the benefit of humanity.© Copyright 2024 IEEE – All rights reserved.
What does the XOR do?
XOR is a bitwise operator, and it stands for ‘exclusive or.’ It performs logical operation. If input bits are the same, then the output will be false(0) else true(1).
By introducing multi-layer perceptrons, the backpropagation algorithm, and appropriate activation functions, we can successfully solve the XOR problem. Neural networks have the potential to solve a wide range of complex problems, and understanding the XOR problem is a crucial step towards harnessing their full power. This problem is significant because it highlights the limitations of single-layer perceptrons. A single-layer perceptron can only learn linearly separable patterns, whereas a straight line or hyperplane can separate the data points. However, they requires a non-linear decision boundary to classify the inputs accurately.
- This non-linearity means that a single-layer perceptron cannot solve the XOR problem, as it can only create linear decision boundaries.
- The XOR operation is a binary operation that takes two binary inputs and produces a binary output.
- There are multiple layer of neurons such as input layer, hidden layer, and output layer.
- Each neuron in a neural network receives several inputs, each input coming with its own weight.
- Backpropagation is a fundamental algorithm used in training artificial neural networks (ANNs).
Neural networks – why everybody has different approach with XOR
Each neuron in the network performs a weighted sum of its inputs, applies an activation function to the sum, and passes the result to the next layer. The backpropagation algorithm is essential for training XOR neural networks, enabling them to learn complex patterns and make accurate predictions. By iteratively adjusting the weights based on the calculated gradients, the network can effectively minimize the error and improve its performance on the XOR task. The hidden layer neurons typically use non-linear activation functions such as the sigmoid or ReLU (Rectified Linear Unit) to enable the network to learn complex patterns. The choice of activation function can significantly affect the performance of the network.
Step 2: Hidden Layer to Output Layer Transformation
This exercise shows that the plasticity of this set of neurons conforming the motif is enough to provide an XOR function. The proposed XOR motif is in fact a simple extension of the well-known lateral inhibition motif, one of the basic core circuit motifs (Luo, 2021). Generate training data with 200 data points using the generateData function.
The XOR function
How many NAND gates are required for XOR?
An XOR gate is made by connecting four NAND gates as shown below. This construction entails a propagation delay three times that of a single NAND gate. , noting from de Morgan's law that a NAND gate is an inverted-input OR gate.
We read every piece of feedback, and take your input very seriously. Stack Exchange network consists of 183 Q&A communities including Stack Overflow, the largest, most trusted online community for developers to learn, share their knowledge, and build their careers.
We have implemented AND, OR, and NAND Gates with the perceptron model. I highly recommend you read my other article on Perceptron neurons before proceeding with this article for better understanding. It works fine with Keras or TensorFlow using loss function ‘mean_squared_error’, sigmoid activation and Adam optimizer. Furthermore weights initialization with random number between 0.5 and 1.0 helps to converge.
Once trained, the neural network should be able to accurately predict the XOR of new inputs it hasn’t seen before. If we change weights on the next step of gradient descent methods, we will minimize the difference between output on the neurons and training set of the vector. As a result, we will have the necessary values of weights and biases in the neural network and output values on the neurons will be the same as the training vector.
Understanding XOR Logic Gate
The second layer (hidden layer) transforms the original non-linearly separable problem into a linearly separable one, which the third layer (output layer) can then solve. And now let’s run all this code, which will train the neural network and calculate the error between the actual values of the XOR function and the received data after the neural network is running. The closer the resulting value is to 0 and 1, the more accurately the neural network solves the problem. Now let’s build the simplest neural network with three neurons to solve the XOR problem and train it using gradient descent. In common implementations of ANNs, the signal for coupling between artificial neurons is a real number, and the output of each artificial neuron is calculated by a nonlinear function of the sum of its inputs.
How many transistors are in XOR?
In the simplest design, only 5 transistors are needed. However in order to send an output 6 transistors will be needed. The XOR gate can be built with NAND gates but 8 transistors are needed. It can also be built with NOR gates and 10 transistors would be needed.
C++ For Sport Improvement: An Entire Information
You also can take a hybrid strategy of breaking the sport into the next stage language for scripting and so forth and then “drop” into C++ land for parts that require the speed and optimizations. My answer could be that it really depends on what you need to do within the video games industry. At the moment if you need to make AAA console games, C++ is a should. No different language will allow you to benefit from the limited sources you’ve on a console. To reply how to learn c++ for game development your particular query, Microsoft will now not be updating XNA, so chances are it won’t be around for much longer. C++ is a nicely established trade normal and won’t be leaving anytime quickly.
Introduction Courses, Objects, And Polymorphism In C++

Learning C++ programming can open up many career Warehouse Automation alternatives in areas corresponding to sport development, embedded techniques, artificial intelligence, and software engineering. While Unity Engine predominantly uses C#, the runtime language for Unity video games is C++, reinforcing the language’s prevalence within the gaming landscape. C++ is a general-purpose, object-oriented programming language that was designed by Bjarne Stroustrup in 1979 to be an extension of the C language. It has the features of imperative, object-oriented in addition to generic programming fashions.
Prime 5 Accounting Software Program For Small Companies In 2024
Keep in thoughts, C++ is a beast of a language, and one e-book is not going to make you a pro overnight. After reading this title, you will nonetheless probably need different resources before you are able to construct your own apps or video games. With gaming particularly, you will probably also need to learn how to use libraries, varied APIs, and so forth. and none of that is lined here. So think of this as merely a light introduction, which will construct a basis your can bring to different extra advanced books.
Superior Graphics And 3d Programming:
Learn the vital thing steps to establishing a subsidiary in Bosnia and Herzegovina, together with understanding local company law and the benefits of establishing there. Discover if AI will exchange developers and what this implies for your corporation. Learn key insights to remain forward in a rapidly evolving tech landscape.
C++ Has Lots Of Library Help

Understand its enterprise influence and why it is important for your firm’s success. Learn how Teamcubate’s expertise can information you in leveraging this technology. Learn the essentials of building a React growth company and harness the facility of top-notch tech solutions with Teamcubate. Discover how using React for your e-commerce website can streamline your business operations, enhance buyer expertise, and drive success. Discover how React, a cutting-edge expertise, can remodel the travel and hospitality industry. Learn from Teamcubate how this revolutionary device can improve your corporation operations and consumer experience.
- If you want a participant to see a sure graphic or message when their character picks up an object, scripting makes that happen.
- On the opposite aspect there are the office/business applications that simply want faster development cycles, stability and to be as extensible as potential.
- This is at a price of lack of capacity to optimize and fine tune how reminiscence and knowledge constructions are used.
- One language that has stood the test of time and remains related at present is C++.
On high of this it is a versatile programming language that gives a decent growth velocity. Portability, efficiency and legacy code bases are the reasons that C/C++ continues to be THE main player in game growth. For a very long time C++ was the lingua franca of the video games trade, however with the advent of the iPhone and Unity it is now possible to make first rate games using languages like C# and Objective-C. I’m not in business yet (I’m 17 years old), but I suppose it’s actually a must to find new languages and applied sciences. Mastering these takes a while (I took me 5 years, so I began on the identical age as you are now), however the expertise you gain is basically superb.
Our guide on C++ developer jobs might help you make informed choices. If you’ve never programmed earlier than, it’s clever to begin studying the fundamentals with a beginner-friendly programming language like Python or Java. You will study important programming ideas corresponding to object-oriented programming and algorithms without having to spend an excessive amount of time worrying about syntax.
Discover how outsourcing SAP growth can streamline your corporation operations. Read on to understand the advantages and the method it results in better project outcomes. Discover how to discover expert SAP builders that may transform your corporation processes and improve your effectivity. Discover how SAP development providers can remodel your corporation operations. Explore the vary of providers available to optimize your processes and drive progress. Learn about SAP Software Developers, their roles, abilities, and the way they can benefit your small business.
C is a viable alternative for recreation improvement as a outcome of its velocity and portability. Beginners can begin game programming in C, as demonstrated by two-player video games where players are assigned O and X. C’s history dates back to 1972, designed by Dennis Ritchie, and it stays relevant in recreation improvement due to its efficiency. While it’s easier to code in strictly high-level programming languages, additionally they come with guardrails that prohibit you from accessing hardware parts.
There are compelling benefits to studying C++ even if you’re not committed to studying game development. C++ is used in numerous AAA video video games and gaming engines for good cause. Its low-level programming abilities offer a high degree of flexibility that simply isn’t available with higher-level recreation programming languages such as Python and C#.
By the tip of the course, you’ll be in a position to develop C++ packages and even apply to C++ jobs with some potential for achievement. No ensures, but this course definitely won’t hurt your probabilities. All in all, there’s a wholesome dose of knowledge obtainable right here, and there are some sources exterior of the standard tutorials on C++ for sport programmers to assist you hone your C++ skills. This has links to the supply code web page, source code snippets web page, C++ ideas web page, and even a “finding a job” page.
Understand their expertise, obligations, and how they contribute to business progress. Discover AI improvement providers for web, app, and game development. In today’s interconnected world, multiplayer functionality is commonly vital function for many games. C++ supplies superior networking capabilities that make real-time multiplayer interactions smooth and lag-free. For games that require fast trade of data packets, C++ is unparalleled in phrases of efficiency.
Firstly it lets gives you entry to 3 units (pc, xbox, zune based) and that is not even including mono xna. The velocity variations are virtually never worth worrying about at this degree and it is just more productive. Of course, most of those features are very helpful, so in C++ you might have to spend a lot more coder time to get the identical outcomes.
However, the skills I gained from learning C++ – notably the low-level stuff, particularly how memory and pointers work – have confirmed invaluable. Now, the 10th purpose to study C++ programming in 2024 is the pay. As you understood the group support of C++, it’s time to move on to the next purpose. The function of C++ programming was to link object orientation to C programming. Major enhancements embody the namespace feature, operator overloading, OOP paradigm, and error and exception handling. Discover how hiring these specialists can drive your business success in right now’s tech-driven world.
Transform Your Business With AI Software Development Solutions https://www.globalcloudteam.com/ — be successful, be the first!
C++ In Gaming: How To Begin Studying
Discover key methods to rent expert SAP developers effectively. Learn tips on how to streamline your hiring process and ensure you select the right talent for your business wants. Explore how SAP methods transform financial administration in businesses. Discover the sensible kotlin application development advantages and efficiency gains SAP brings to finance departments. Explore important practices for hiring an AI developer and discover ways to identify the perfect match for your corporation wants.
React Growth Companies: Enhancing Your Small Business Within The Digital World
C++ stands out as a high-performance programming language famend for its object-oriented paradigm. Particularly acclaimed for growing large-scale products, C++ is an extension of the C language and lays the inspiration for languages like Java. Although writing C++ code could demand extra time, the payoff lies in its unparalleled performance. Investing time in mastering the fundamentals of C++ in game growth is a strategic endeavor. Also, C++ Developers are quite sought they usually hold a few of the most high-paying jobs in the trade with a mean how to learn c++ for game development base pay of $103, 035 per 12 months. This web site has tutorials for getting began with C and C++.
Recreation Improvement In C++ For Newbies
It’s the language behind in style games like Angry Birds and Age of Conan, and it powers engines like CryEngine, Gideros Mobile, and Corona SDK. The power of C++ when it comes to recreation growth is the flexibility to exactly structure the data-structures that your software program will use. When performant real-time systems (such as games) began rising, it was the most generally supported and most developed programming language. As such it was a natural selection for video games that attempt to push platforms to their limit. This has in time period lead most builders to go alongside with this choice even if they need it or not. It permits developers to create high-performance software that can be utilized in quite so much of industries.
What’s A Full Stack Sap Developer? – Essential Information For Business Leaders
While machine code have to be translated from higher-level languages. It does take a little bit longer to write down C++ code than it does to write down code in high-level languages, however this may be a truthful sacrifice for effectivity. Learning Python also makes it easier to use GDScript, the programming language for the popular recreation engine Godot. GDScript’s creators built it to mimic Python’s readability and beginner-friendly syntax, while also providing features specific to gaming.
How To Hire An Sap Developer: Important Tips For Fulfillment
But it could be helpful to check it out anyway, I suppose it is pretty neat even with my restricted understanding of its ideas. You seem to have reasons not to learn C++, I assume you might be truly simply making an attempt to rationalize your wish to not be taught one thing new. Also, the syntax of C, C++, and Java are almost the same, so learning Java and C after C++ shall be very easy. Start by familiarizing yourself with the engine’s interface, basic options, and workflow. Both engines have intensive documentation and tutorials for novices. A fairly broad issue, game creation may be tackled in a selection of methods.
This is among the major causes that applications requiring multi-platform or multi-device improvement usually use C++. A lot of internet browsers are developed utilizing C++ similar to Chrome, Firefox, Safari, and so on. Chrome incorporates C++ in the rendering engine, JavaScript engine, and UI. Firefox uses mainly within the rendering engine and slightly within the UI.
Unity can also be a popular recreation engine for VR games—90% of all Samsung Gear and 53% of Oculus Rift VR games use Unity. If you need to create games in Unity or for VR, C# must be in your toolbox. The good news is that job growth for C++ coders has remained stable at 8% per 12 months. Before you dive into studying a new language you might be wondering what you’ll be capable of build when you grasp the language, or if it’ll still be in use 10 years from now.
One of the biggest benefits of C++ programming is its cross-platform compatibility. C++ code can run on different #operatingsystems , together with Windows, Linux, macOS, and cellular platforms. This signifies that builders can write code as quickly as and have it run on totally different platforms without making vital adjustments. C++ with DSA Course by Physics Wallah is ideal for learning C++ game improvement abilities.
Here’s why, say you decide c++, well nice but what api are you going to make use of to draw? Both C++ and C# belong to the C language family, sharing basic traits but differing in essential aspects. At some level we have to ask our selves is it purely C++ giving us the highest notch speeds in body charges. Language barrier is only wrapped round its tooling, C++ has nothing standing in its method.
In this tutorial, you will learn concerning the C++ language and understand the top 10 causes to be taught C++ in 2024. In addition to the flexibleness that comes with its low-level parts, C++ maintains excessive efficiency as a end result of it compiles down to machine code. Because of this, C++ programs can run at almost the speed of the machine. On the other hand, higher-level languages require translation into machine code.
- In fact, Bjarne Stroustrup, the creator of the language, put collectively an extended listing of C++ functions.
- Anyway, it is a utterly free website that guides you on tips on how to learn C++.
- Just those two factors alone make it reasonable to stick with C++.
- Learn simple and effective methods to enhance your small enterprise cash move.
- Learn how Teamcubate’s experience can information you in leveraging this expertise.
It’s no secret that C++ is doubtless certainly one of the most widely used programming languages right now. Embarking on the journey of C++ recreation growth requires a structured roadmap to guide you thru the intricate world of creating interactive and fascinating video games. Whether you’re a novice or an experienced developer, this roadmap outlines the key milestones and skills to grasp for a profitable venture into C++ recreation growth.
Don’t worry about forgetting the details, should you stop using C++ for some purpose (or XNA or something else). And you’ll be able to pick up the small print once more easily if you want to. Additionally, there have been several events the place I’ve needed to learn other folks’s C++ code. If you understand how to program in C# or Java you’ll find a way to probably guess what’s going on – however knowing is a lot better. As you understood the Embedded techniques, move to yet another excuse.
Its recognition is not the reason it’s nice for recreation growth, though. Although Python is a powerful programming language, what it positive aspects in usability, growth time, and readability, it loses in velocity. Python runs more slowly than other programming languages like C++, and it isn’t a traditional online game scripting language like C#. However, for newcomers, Python is among the finest starter programming languages—and recreation engines like Godot are basing their native scripts on Python to make it simpler to program.
You do have to be laptop literate, however you don’t have to have programming expertise. You may wish to give the free tutorial a stab before you go dropping money on an e book. Or return and check out the LearnCPP tutorial firstly of this guide earlier than tapping into the tutorial at Cprogramming. It’s a lacking article here or there, or an inverted phrasing–the kinds of slipups that come with studying English as a second language, and getting fairly dang close to mastering it.

Transform Your Business With AI Software Development Solutions https://www.globalcloudteam.com/ — be successful, be the first!
