How dancing can supercharge your health after 55: Discover why ballroom beats the gym!
Team Metabolic Health
Researchers highlight how group dance, from ballroom to folk styles, enhances well-being and fitness in older adults, advocating for more inclusive and well-reported studies to support diverse communities.
In a recent study published in the journal PLOS One, researchers reviewed dance programs’ range, scope, and effectiveness in improving the health and well-being of older adults. The study provides a detailed analysis of how different dance styles contribute to various health outcomes, highlighting the distinct benefits associated with each type of program.
Researchers noted that creative and dance movement therapy (DMT) programs consistently delivered emotional and social benefits, enhancing mental well-being, particularly in older adults who might be less inclined to engage in traditional exercise.
Research interest in the health benefits of cultural activities and arts has exponentially grown over the past decades. Dancing is recommended as an exercise for older adults. Group dance participation offers an accessible, effective, and sustainable means to promote health. Nonetheless, the lack of theoretical foundations and methodologies and inconsistent outcomes across studies have introduced challenges in meaningfully interpreting and applying the findings. The authors stress the need for more theory-driven research and clearer reporting standards to advance the field.

Study: The use of dance to improve the health and wellbeing of older adults: A global scoping review of research trials. Image Credi: SeventyFour/Shutterstock
About the study
In the present study, researchers performed a scoping review to explore the use of dance in improving the well-being and health of older adults. They searched the Web of Science, PsycINFO, CINAHL Plus, Embase, and MEDLINE databases for studies that evaluated the benefits of dance programs on the health and well-being of older adults aged ≥ 55.
Studies involving older adults with specific health conditions or rehabilitation were excluded. Search results were deduplicated, followed by the screening of titles/abstracts and full texts. The following data were extracted: study details, trial context, participant characteristics, characteristics and delivery of dance programs, outcomes, and comparator types and activities. The study also looked into how participant demographics, including age, gender, and socio-economic status, impacted participation and outcomes.
The template for intervention, description, and replication (TIDieR) tool was used to categorize the delivery and characteristics of dance programs. The stratification of well-being and health outcomes was based on the taxonomy of the core outcome measures in the effectiveness trials database. Data collation involved classifying and standardizing program features and identifying and consolidating recurrent features from each TIDieR category.
Data synthesis involved narrative and numerical summaries, descriptive statistical analysis, and evidence mapping of dance health trial reporting. A TIDieR item or program feature was considered “reported” if comprehensively and clearly described, consistent with accepted standards, “partially reported” if incomplete information was provided, and “not reported” if no/limited information was available.
Findings
Dancing improves cardiovascular health, enhancing heart and lung function while reducing the risk of cardiovascular disease—key benefits for older adults engaged in dance programs.
Database searches identified more than 7,000 studies. Of these, only 148 articles met the eligibility criteria and were included. The earliest trial was published in 1980, and the publication frequency increased through the mid-2000s. Most studies (50.7%) were randomized controlled trials (RCTs), followed by non-RCTs (20.3%), evaluation trials (14.2%), and qualitative studies (8.8%), among others. Recent years have seen an increase in mixed-method approaches, integrating both qualitative and quantitative data for a more comprehensive analysis.
Mixed method approaches were more common in the past decade. The 148 studies evaluated 115 trials with 8,060 participants, with a mean of 70 participants per trial. Around 68% of trials were conducted in the community, and 96% of programs were delivered live, in-person. Most trials were open to adults in late middle age, and 33 trials recruited adults aged ≥ 85.
Twenty-two dance programs were designed for females, and 29 trials recruited only females. No trial was designed for males, and 70% of trials had mixed-gender groups. Moreover, most participants were females, with mixed-gender trials having 75% female participation, on average. Only seven trials were offered to low-income participants, with only two in remote/rural settings. This gap underscores the need for more inclusive research targeting underserved populations.
Around 21% of trials required prior dance experience for inclusion. Dance program genres/styles were categorized as 1) modern and traditional forms of folk, social, or national dances, 2) mixed dance styles, 3) formal dance styles from the Global North and South, 4) ballroom dance, 5) aerobic exercise dance, 6) dance movement therapy (DMT), and 7) creative dance programs. Ballroom and folk dance styles, in particular, showed the most consistent physical and emotional benefits.
Dance enhances bone health and reduces osteoporosis risk, an important benefit for older adults seeking to maintain physical stability and strength through enjoyable activities.
A clear, rational goal/theory for the dance program was reported in 67.8% of trials and partially reported in 22.6%. Rationales for dance programs were diverse and included dance as an exercise, particularly in those who do not exercise, dance as an activity to promote creative aging, dance for preventing falls, and dance as a low-cost, inclusive, fun, popular, and sustainable activity, among others. The diversity of motivations suggests that dance can be tailored to meet various physical, cognitive, and social needs of older adults.
Six studies evaluated previously piloted programs, 12 examined pre-existing programs, and the remainder assessed new dance programs. Notably, only seven trials involved older adults in developing dance programs. Involving participants in the design phase could improve program relevance and adherence. Thirty-two trials reported the physical intensity of dance programs, and 17 partially reported it. Trials usually offered 60 minutes of group dancing, two/three times per week, for 12 to 16 weeks.
The expertise of dance program facilitators was reported in 85 trials and partially reported in five trials. Program facilitators received training in only 16 trials. Program adherence was recorded for participants of group dancing and reported in 48 trials and partially reported in four trials. Attendance rates were similar across programs with two or three weekly sessions but were lower in longer programs. This highlights the challenge of sustaining engagement in extended dance interventions.
Only 28 trials reported program safety; two were described as safe, three reported no serious adverse events, 15 reported no adverse events, and two reported no injuries. Six trials reported one adverse event. Motor and physical functioning was the most prominent outcome assessed in 80 trials, which significantly improved in 48.5% of conducted tests.
Cardiovascular strength and endurance were investigated in 48 trials. Significant improvements in this domain were noted in 60.2% of tests. Metabolic and physiological outcomes were assessed in 28 trials, with improvements in about 30% of tests. Twenty-seven trials evaluated executive and cognitive functioning, with positive benefits observed in only 16.4% of tests. Despite limited cognitive gains, emotional and social benefits were consistently reported, especially in creative and folk dance programs.
Ballroom dance consistently showed the most positive results across outcome domains, achieving better physical functioning and cardiovascular strength and endurance outcomes than aerobic exercise dance. Folk, social, or national dance and DMT/creative dance resulted in consistent emotional well-being and mental health benefits. Dance was frequently compared with daily living or usual care. Sometimes, group dance was compared to educational, arts, or social activities. These comparisons underscore dance’s potential to offer holistic health benefits beyond standard physical exercise.
Conclusions
This scoping review mapped the range, scope, and efficacy of dance health programs for older populations. Dance programs showed substantial variations across factors likely to influence participation and health outcomes. Program success also varied across dance styles and health domains. Dance is a safe, meaningful, and low-cost health resource for older people. The authors recommend prioritizing more inclusive research designs, particularly those that engage underserved and underrepresented groups. Future research should improve access for underserved groups, incorporate practitioner and participant insights, and enhance engagement and adherence.
To ensure robust evidence synthesis, clearer standards for program reporting are needed. This will facilitate comparisons across studies and contribute to more effective program designs in the future.
Credit- news-medical.net
How your baby’s birth and environment can shape lifelong gut health
Team Metabolic Health
New research shows how birth delivery methods and natural surroundings impact infant gut health, emphasizing the critical role of outdoor time in shaping healthy gut diversity as babies grow.
In a recent study published in the journal Environment International, researchers in Finland analyzed the influence of early life factors in shaping the community composition of gut microflora during infancy. High-throughput sequencing alongside multiple metrics of residential greenery revealed the significant role of green environments in determining infants’ gut diversity, particularly during early infancy.
The study found that infants delivered via cesarean section showed differences in gut bacterial diversity compared to those born vaginally, impacting the initial microbial colonization.
However, the study found that this association was limited to alpha diversity, which measures species richness and diversity, rather than specific microbial community composition. Surprisingly, no such association between residential proximity to green environments and gut floral populations could be established during late infancy. Instead, gut microbial communities were more strongly determined by the time spent outdoors. Notably, birth mode and the presence of siblings were demonstrated to influence infant diversity to substantially greater extents.
These findings help inform pediatricians and (prospective) parents of the early life factors that, despite appearing seemingly disconnected, can have profound and potentially lifelong impacts on their children’s health.

Study: The role of early life factors and green living environment in the development of gut microbiota in infancy: Population-based cohort study. Image Credit: Design_Cells/Shutterstock
Background
The recent global surge in the prevalence of chronic, non-communicable diseases is partially attributed to the influence of environmental factors and behavioral decisions on gut microbial health. A growing body of evidence links the benefits of ‘healthy’ dietary patterns (e.g., Mediterranean diet) to gut diversity and community composition improvements.
While improvements in diet and other health behaviors can benefit current life gut health, research suggests that the foundations of lifelong gut health are established at birth. The initial gut floral inoculum, primarily derived from infants’ placental connection to their mothers, may be subject to considerable environmentally-mediated variation during early to late infancy, thereby setting the foundation for future gut microbial health.
Unfortunately, most conventional gut microfloral investigations have been carried out on adults. The handful of infant-centric gut microbial studies suffer from the almost ubiquitous demerit of focusing on a single factor (e.g., birth mode or the presence of pets) rather than the holistic and potentially multifaceted impacts of multiple simultaneously acting influences.
About the study
The present study had three main aims: First, to explore the maturation of gut flora across infancy; second, to identify the environmental influences that alter microbial community composition during early and late infancy stages; and third, to investigate associations between metrics of residential greenery and infant gut microbial health.
Study data was obtained from the Steps to Healthy Development of Children (STEPS), a longitudinal cohort comprising Finnish- and Swedish mothers who delivered babies between 2008 and 2010 in a specific Finnish hospital (Hospital District of Southwest Finland). A subset of this 14,946 infant-strong cohort called the ‘intensive follow-up group’ was included as participants in the present investigation. Participants were divided into ‘early’ (0.5-5 months) and ‘late’ (11-17 months) subcohorts.
Alpha diversity, a key measure of microbial richness, was significantly higher in infants exposed to more natural environments during early infancy, highlighting a potential window of opportunity for environmental influence.
Data collection included parent/guardian-provided socioeconomic, demographic, and medical records and 1,823 fecal samples for sequence-based infant gut microbiota characterization. Qiagen reagents and protocols were used to extract DNA from fecal samples, and the Illumina MiSeq v3 platform was used for 16S metagenomic sequencing. Reads thus obtained were processed (cleaned and assembled), following which infant-specific microbial community composition was established using the Silva 138.1 prokaryotic SSU taxonomic database.
Additional early life factor data (birth type, gestational age at birth, breastfeeding status, birth weight) were obtained from medical health records and parent-completed follow-up questionnaires. The Population Register Center data for each household was used in tandem with Geographical Information Systems (GIS) data to measure residential vegetation indices – VCDI (an index of vegetation classes) and NI (an index of human land use).
Study findings
The included infant cohort comprised 892 early and 931 late infants, 52% of whom were boys and 46% of whom had older siblings. Over half of the participants’ households were located in non-natural (urban) areas. However, vegetation cover was observed to be moderate or high in most instances. Birth mode data revealed that 11% were delivered via cesarean section, and approximately 10% received maternity hospital-administered antibiotics shortly following delivery.
Surprisingly, while greenery around the home had a limited impact during late infancy, it played a notable role in early infancy, suggesting that timing of exposure to natural environments is crucial for influencing gut microbiota diversity.
Analyses of the variables influencing infants’ gut community composition revealed age to be a major determinant. Comparisons between early and late cohorts revealed the former to be dominated by Actinobacteriota (54 %) and substantially more variable than the latter (Firmicutes [59 %]), highlighting that age alone was responsible for explaining around 9% of cohort-wide variation. Previous investigations in the field have rarely included infant-specific age subcohorts, often considering 0-3 years as a single age category. These findings suggest future research needs to account for age subclasses in infant-centric study models.
The analysis showed that birth mode, presence of siblings, and maternal age were the strongest contributors to infants’ gut microbial assemblages. While family income, breastfeeding status, perinatal antibiotic exposure, and outdoor time were significant associations with the gut microbiota, their associations were comparatively weaker.
According to the study’s adjusted models, in early infancy, birth mode (cesarean/vaginal) accounted for 0.5% of the variation in gut microbiota community composition, gradually decreasing to 0.3% in late infancy. The presence of siblings became a more significant factor during late infancy, explaining 0.7% of variability compared to 0.5% in early infancy. Overall, siblings were associated with an increase in gut microbial diversity in both age groups.
Surprisingly, while residential greenery measures established a link between green environments and gut flora, this interaction was primarily limited to early infancy and involved only alpha diversity measures, such as species richness. In contrast, outdoor exposure was a more important predictor of microbiota composition during late infancy.
Conclusions
The present study identifies the factors determining gut microbial diversity during early and late infancy stages and measures their relative impacts. It identifies birth mode, presence of older siblings, and maternal age as the most influential factors, highlighting their roles in shaping the presence and relative abundances of different bacterial populations. Additionally, family income, breastfeeding status, perinatal antibiotic exposure, and outdoor time were found to exert weaker influences on gut flora.
“Moreover, our analysis revealed that associations between residential green environment and gut microbiota alpha diversity were more pronounced in early infancy than in late infancy, indicating a critical period of susceptibility to environmental influences on gut microbiota diversity,” the authors concluded. This underscores the importance of a holistic understanding of early environmental and familial influences on children’s health.
Credit: news-medical.net
Heart blockage: 7 tips to ensure your arteries are clean
Team Metabolic Health
There are natural ways such as a healthy diet and exercise to prevent heart blockage, and even reverse the damage.
A heart blockage is not a death sentence if caught in time and managed responsibly. It is possible to reverse a heart blockage and unclog your arteries with the help of simple lifestyle changes. The blood in our body flows through our arteries, and when these arteries are blocked, due to plaques of cholesterol, fats, and other substances, they become narrow. Changes such as weight control, stress reduction, a well-balanced meal, and adequate exercise, besides your heart medications, can help dissolve heart blocks and restore complete blood flow. A regular check on your blood pressure as well as cholesterol levels can also help you seek treatment on time, and minimise the damage.

A good diet and moderate exercises can help to keep your heart healthy. Image courtesy: Adobe Stock
What is a heart blockage?
A heart blockage, commonly referred to as coronary artery disease, occurs when the arteries that supply blood to the heart become narrowed or obstructed. “This blockage is primarily due to the accumulation of fatty deposits, cholesterol, and other substances, forming plaques in the artery walls. Over time, these plaques can harden or rupture, leading to reduced blood flow to the heart muscle,” explains cardiologist Dr Chandrashekhar Kulkarni. As a result, individuals may experience symptoms such as chest pain, known as angina, shortness of breath, or even more severe complications like heart attacks, where the heart muscle suffers damage due to insufficient blood supply. Check out the signs of a healthy heart here.
What are the causes of a heart blockage?
Several factors contribute to the development of heart blockage. The most prevalent cause is atherosclerosis, a condition that happens due to the buildup of fatty plaques in the arteries. “This buildup narrows the arteries and restricts blood flow. High blood pressure is another significant factor; it can cause damage to artery walls over time, making them more susceptible to plaque accumulation,” explains Dr Kulkarni. High cholesterol, particularly elevated levels of low-density lipoprotein (LDL), promotes plaque formation.
Besides this, conditions such as diabetes can further complicate this scenario, as high blood sugar levels can damage blood vessels and accelerate atherosclerosis. The World Health Organization (WHO) states that an unhealthy diet, physical inactivity, tobacco use and excessive alcohol are some of the biggest causes of heart disease. Lifestyle choices such as smoking are detrimental, as tobacco use damages the arterial lining and increases plaque buildup. Obesity contributes to heart blockage by raising cholesterol levels, blood pressure, and the likelihood of developing diabetes. A sedentary lifestyle increases the chances of these risks, while genetic predisposition can make individuals more susceptible to heart disease. Finally, age plays a crucial role; as individuals get older, the risk of developing heart conditions increases significantly.
What are the signs of a heart blockage?
While it is very difficult to detect a heart blockage without a medical test, there are a few warning signs that can help you. A certain heaviness in the chest is usually the first sign, followed by a choking sensation and a feeling of being unwell. A family history of heart problems should also keep you on your toes, and you must get checked regularly. Check out the other signs of a blocked artery here.
What are the different types of heart blockages?
Heart blockages can be classified based on their severity. There are three levels of blockages:
First-degree heart block: This is the first level of blockage, and might not require much medical treatment. Patients can lead a life without any symptoms at this level. It is detected in an ECG.
Second-degree heart block: Here, some electrical signals don’t reach all the chambers of the heart. You might need a pacemaker to help your heart beat at a normal rate.
Third-degree heart block: In this stage there is no communication between the ventricles and the atria. This is the most severe level. It can even become a medical emergency.
Can you prevent a heart blockage naturally?
Yes, heart blockage can often be prevented naturally through a combination of lifestyle changes. The UK’s National Health Services (NHS) states that a healthy diet, followed by being more physically active and keeping your weight in check can help prevent a heart blockage. Focusing on heart health through diet, exercise, and other healthy habits can significantly reduce the risk of atherosclerosis and related complications, says Dr Kulkarni. Adopting a proactive approach to heart health allows individuals to take charge of their well-being, potentially avoiding serious health issues in the future.
How to prevent a heart blockage naturally?
Preventing heart blockage involves several key strategies. Here is what you should do:
1. Eat right
The first step is maintaining a healthy diet. A diet rich in fruits, vegetables, whole grains, and healthy fats, such as those from fish, nuts, and olive oil, helps lower cholesterol levels and blood pressure. Check out the important heart-healthy vitamins and minerals, and make sure to include these in your diet.
2. Get moving
Engaging in regular exercise is vital. Aim for at least 150 minutes of moderate aerobic activity each week. Activities such as walking, jogging, swimming, or cycling strengthen the heart and improve circulation. The US National Heart Lung and Blood Institute states that moderate- and vigorous-intensity aerobic activity can strengthen the heart muscle. This helps the heart to pump blood more effectively.
3. No Smoking
Third, quitting smoking is crucial. Tobacco use is a leading risk factor for heart disease, and cessation can drastically improve cardiovascular health. A study, published in the Journal of the American College of Cardiology, shows the association between smoking and an increased risk of atherosclerotic diseases after smoking cessation.
4. Manage stress
Managing stress through techniques like meditation, yoga, or deep breathing can mitigate its negative effects on the heart. A study, cited by the American Heart Association, concluded that stress-reducing transcendental meditation led to a 48 percent reduction in the risk of mortality, myocardial infarction, and stroke.
5. Monitor blood pressure and cholesterol.
It is important to monitor blood pressure and cholesterol levels regularly. Early detection of any issues allows for timely intervention through lifestyle changes or medical treatment. Check out these telltale signs of low blood pressure that you should never ignore.
6. Keep your weight in check
Maintaining a healthy weight through balanced nutrition and exercise is key, as excess weight is associated with various heart disease risk factors. The American Heart Association states that obesity promotes the buildup of plaque inside artery walls. It can also cause high blood pressure.
7. Avoid alcohol
Limiting alcohol intake is advisable. While moderate consumption may have some benefits, excessive drinking can lead to elevated blood pressure and other health complications. The American Heart Association states that one drink a day for non-pregnant women and two drinks a day for men is the upper limit of alcohol consumption, and this should not be crossed.
What to eat to avoid heart blockage?
A heart-healthy diet consists of a variety of nutrient-dense foods that promote cardiovascular health. This includes the following:
Fruits and vegetables are high in vitamins, minerals, and antioxidants that protect the heart.
Whole grains, such as brown rice, quinoa, and oats, provide fibre, which helps lower cholesterol levels.
Healthy fats, like those found in avocados, nuts, seeds, and fatty fish (such as salmon), are crucial for reducing bad cholesterol and inflammation.
Lean proteins, including chicken, turkey, beans, and legumes, while limiting red meat and processed meats.
A diet low in sodium can help manage blood pressure.
Overall, this balanced approach supports heart health and helps prevent the development of blockages, says Dr Kulkarni.
Exercises to prevent heart blockage
Effective exercises for preventing heart blockage include a combination of aerobic and strength-training activities.
Aerobic exercise, such as walking, jogging, swimming, or cycling, is particularly beneficial as it strengthens the heart, improves circulation, and helps maintain a healthy weight.
You can also include weights or using resistance bands. These also play an important role in building muscle, increasing metabolism, and supporting overall cardiovascular health.
Additionally, incorporating flexibility and stretching exercises, such as yoga or Pilates, can enhance overall fitness and promote stress management.
By combining these various forms of exercise, individuals can create a comprehensive fitness routine that effectively supports heart health and reduces the risk of blockages.
Credit: healthshots.com
Les Effets Secondaires des Stéroïdes Anabolisants
Les Effets Secondaires des Stéroïdes Anabolisants
Les stéroïdes anabolisants, bien que souvent utilisés pour améliorer la performance sportive et augmenter la masse musculaire, comportent de nombreux risques pour la santé. Il est essentiel de comprendre les effets secondaires des stéroïdes anabolisants avant de décider d’en faire usage.
Les Effets Physiques
Les effets secondaires physiques peuvent varier d’une personne à l’autre, mais incluent généralement :
- Augmentation de la pression artérielle
- Problèmes cardiovasculaires (risque accru de crises cardiaques et d’ AVC)
- Modification du cholestérol (augmentation du LDL et diminution du HDL)
- Acné et problèmes de peau
- Retenue d’eau et gonflement
- Changements dans la libido
Effets sur le Système Endocrinien
Les stéroïdes anabolisants peuvent également perturber le système endocrinien, entraînant :
- Atrophie testiculaire chez les hommes
- Menstruations irrégulières chez les femmes
- Développement excessif des seins chez les hommes (gynécomastie)
- Risque accru de troubles hormonaux
Les Effets Psychologiques
En plus des effets physiques, les effets secondaires des stéroïdes anabolisants https://steroidesfr24.com/ peuvent être psychologiques :
- Augmentation de l’agressivité
- Dépression et sautes d’humeur
- Dépendance psychologique
- Modifications de l’estime de soi
Impact sur la Santé Mentale
Il est important de noter que l’utilisation abusive des stéroïdes peut conduire à des problèmes de santé mentale, y compris :
- Anxiété
- Paranoïa
- Comportements obsessionnels
FAQs sur les Effets Secondaires des Stéroïdes Anabolisants
Quels sont les signes d’une utilisation abusive de stéroïdes ?
Les signes incluent une hypertrophie musculaire rapide, des changements d’humeur extrêmes, et des problèmes de peau comme l’acné sévère.
Est-il possible de reverser les effets secondaires des stéroïdes ?
Dans certains cas, une cessation de l’utilisation peut permettre aux effets secondaires de s’estomper, mais certains dommages, notamment ceux au cœur ou au foie, peuvent être permanents.
Qui est le plus susceptible d’expérimenter ces effets secondaires ?
Les utilisateurs de stéroïdes anabolisants, en particulier ceux qui commencent à un jeune âge ou qui en abusent, sont les plus susceptibles de ressentir des effets secondaires graves.
Conclusion
Bien que les stéroïdes anabolisants puissent offrir des résultats rapides en termes de performance physique et de développement musculaire, les effets secondaires des stéroïdes anabolisants sont importants et souvent dangereux. Il est crucial d’évaluer soigneusement les risques avant d’envisager leur utilisation.
People in Punjab spend more from pocket for treatment, reveals survey
Team Metabolic Health
Despite the govt’s efforts to reduce out-of-pocket healthcare expenses, people in Punjab bear a substantial portion of costs directly at the point of treatment. This indicates a heavy reliance on out-of-pocket payments.
Alarmingly, Punjab has one of the country’s highest out-of-pocket healthcare expenditure rates, surpassing the national average. To meet medical expenses, the people are forced to either deplete their savings or resort to borrowing. In Punjab, the average medical expenditure for hospitalised treatment over the last 365 days was Rs 8,306 for rural households, compared to Rs 8,272 for urban households, according to the Comprehensive Annual Modular Survey conducted for the period between July 2022 and June 2023 by the ministry of statistics and programme implementation.
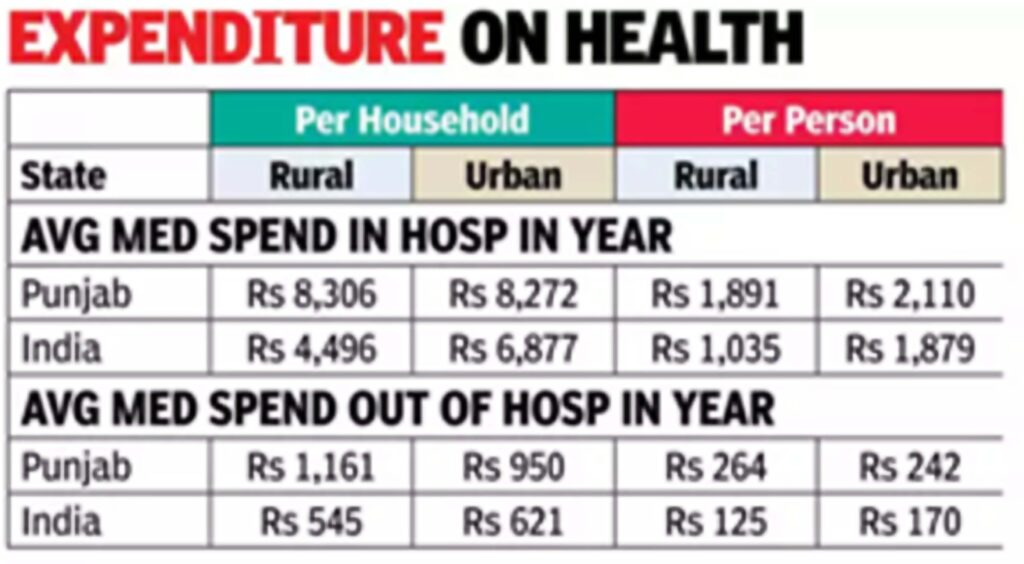
At Rs 2,110, per person expenditure on hospitalised treatment, however, was higher in urban areas as compared to Rs 1,891 in rural areas. For non-hospitalised treatment over the last 30 days, the average medical expenditure per household was Rs 1,161 in rural areas and Rs 950 in urban areas, while per person expense was Rs 264 in rural areas and Rs 242 in urban areas. The average out-of-pocket medical expenditure per household on hospitalisation over the last one year was Rs 7,374 in rural areas and Rs 6,963 in urban areas, compared to the national average of Rs 4,129 in rural areas and Rs 5,290 in urban areas. The average per person out-of-pocket expense stood at Rs 1,679 in rural areas and Rs 1,776 in urban areas. Additionally, the average out-of-pocket medical expenditure per household on non-hospitalisation over the last one month was Rs 1,139 in rural areas and Rs 916 in urban areas, against the national averages of Rs 539 and Rs 606, respectively.
To determine the total health expenditure incurred by households, the survey collected data at disaggregated levels across various components, including package and non-package expenses such as doctor’s fees, medicine costs, diagnostic tests, bed charges, other medical expenses, and transport expenses. Expenditures were recorded when initially borne by the patient’s household, regardless of whether they were reimbursed later.
Prof Aswini Kumar Nanda, department of economics, Central University, Jammu, attributed the high out-of-pocket expenditure on healthcare to heavy reliance on private health facilities. This is largely due to inadequate public health services, he said.
Even in areas where public health facilities exist, people often choose private facilities due to better services and health insurance coverage, Prof Nanda explained.
Since insurance coverage is generally insufficient to cover all expenses, especially for chronic diseases like cancer, people end up paying out of pocket. For financially vulnerable individuals, this can lead to dire consequences, such as forgoing essential treatment or resorting to desperate financing options. “Improving public healthcare by enhancing the coverage and quality of services can help reduce out-of-pocket spending,” said Prof Nanda.
Credit: The Times of India
Nvidia-Backed AI Firm Unveils Drug Discovery “Breakthrough”
Team Metabolic Health
A growing number of tech startups are using AI to advance pharmaceutical research. Iambic, which has previously won investment from tech giant Nvidia, published details of its new AI drug discovery model, named “Enchant”.
The company said its model set a new benchmark, with a 0.74 accuracy prediction score.
Biotech firm Iambic Therapeutics unveiled on Tuesday what it says is a breakthrough artificial intelligence model that could drastically reduce the time and money needed to develop new drugs.
A growing number of tech startups are using AI to advance pharmaceutical research. Iambic, which has previously won investment from tech giant Nvidia, published details of its new AI drug discovery model, named “Enchant”.
Enchant was trained on large troves of pre-clinical data, derived from laboratory tests conducted on drugs before they were ever tested on humans. The model has been designed to predict how a given drug will perform at the earliest stage of development.
In a white paper published by Iambic, Enchant showed a high degree of accuracy when predicting how well the human body would absorb certain drugs, with results cross-referenced to real-world outcomes.
The company said its model set a new benchmark, with a 0.74 accuracy prediction score. By comparison, earlier models had only achieved as high as 0.58.
Iambic co-founder and chief technology officer Fred Manby told Reuters that researchers using Enchant could potentially halve the investment needed to develop some pharmaceuticals, as they could see how successful a drug is likely to be at the earliest stage.
“The cost of getting a product to market is often quoted at around $2 billion, and a lot of that isn’t about the programme costs, but the failure rates. The costs of getting a product all the way to a marketed medicine derive from a high chance of late-stage failure,” he said.
“If you make a 10% improvement in each stage of clinical development, you would basically halve the cost, because it applies cumulatively.”
Frances Arnold, who won the chemistry Nobel Prize in 2018 and sits on Iambic’s board, told Reuters the development represented a major advance in the use of AI for drug discovery.
Citing Google DeepMind’s AlphaFold program, which recently won its developers the chemistry Nobel Prize, Arnold said Enchant addressed a different challenge in the drug discovery pipeline.
“AlphaFold predicts the 3D structure of how a molecule binds to a protein target, but structure is not enough,” she said.
“The success of a drug candidate is determined by its pharmacokinetic, efficacy, and toxicity properties. Enchant addresses these distinct and important challenges.”
Credit: NDTV
Think tonsillitis is just for kids? Think again
Team Metabolic Health
Just about every child gets tonsillitis at least once. But sore, red, inflamed tonsils can happen to anyone, including adults of any age. Here’s what you need to know about tonsillitis symptoms, treatment, and self-care methods you can use at home for much-needed relief.
What is tonsillitis?
Tonsillitis is inflammation and swelling of the tonsils, the two round or oval, slightly pinkish lymph glands in the top back part of your mouth.
These glands help prevent viruses and bacteria from infecting you. But when an infection takes hold in the throat, it can cause your tonsils to swell. By far, the most common bacterial cause of tonsillitis is Streptococcus (known as strep throat).

Symptoms of tonsillitis
Common tonsillitis symptoms include: difficulty or pain with swallowing, sore throat, fever
visible redness or swelling in the back of the mouth, swollen lymph glands in the neck, white or yellow patches or pus on your tonsils, bad breath, breathing through your mouth or snoring, feeling tired or lethargic.
Any throat infection can lead to swelling of the tonsils. Reasons to suspect strep throat is the likely cause are a very sore throat, marked difficulty swallowing, fever, and body aches along with tonsillar swelling.
Acute versus chronic tonsillitis
The symptoms of acute tonsillitis usually come on suddenly, with the onset of an infection, then go away after a few days to one week. Symptoms of chronic tonsillitis or recurrent tonsillitis linger for weeks, or resolve but come back repeatedly.
Experts don’t yet understand what makes some people more likely to develop chronic tonsillitis or recurrent tonsillitis.
If you have chronic tonsillitis, you might feel like your sore throat never goes away. The lymph nodes in your neck may remain tender to the touch, and you might notice debris on your tonsils called tonsil stones. Tonsil stones look like small white or yellow pebbles and may cause bad breath in addition to a sore throat.
In some severe (but rare) cases of tonsillitis, adolescents and adults may develop what’s called a peritonsillar abscess, a pocket of pus within one tonsil. This can make your sore throat even worse. It can also cause drooling, trouble opening your mouth, or changes in the sound of your voice.
Diagnosing tonsillitis
Call your doctor’s office or go to urgent care if you have sudden onset of a very sore throat, fever, body aches, and marked pain or difficulty when you swallow. Otherwise, you can call for advice if symptoms persist or are getting worse over the next two to three days.
If you do need medical evaluation, the clinician will start by asking about your symptoms and health history. They will examine your throat looking for inflammation and redness, and check both sides of your neck for swelling or tenderness.
Most likely, the clinician will perform a rapid strep test with a result available while you are in the office. If it is positive, the clinician will prescribe antibiotics. You can have strep throat with a negative rapid test. If your symptoms and throat exam are highly suggestive of strep, the clinician will send out a culture and may choose to still recommend antibiotics.
Adolescents and adults may also be tested for certain sexually transmitted infections that could cause tonsil swelling.
Treating tonsillitis
Your test results help determine the best tonsillitis treatment for you. If you have strep throat, you’ll be prescribed an antibiotic to fight the bacterial infection. You’ll usually start to notice your symptoms improve within two to three days of starting the antibiotics.
If your doctor thinks it’s more likely you have a viral infection, you won’t be prescribed antibiotics. Your doctor might recommend over-the-counter treatments to manage throat discomfort.
Treating chronic tonsillitis
Surgically removing the tonsils used to be more common. Now, surgery is typically only recommended for people with chronic tonsillitis or many episodes of recurrent tonsillitis. Called a tonsillectomy, the procedure doesn’t require a hospital stay. An otolaryngologist, or ear, nose, and throat specialist, will help determine if you’re a good candidate for tonsil removal.
If you develop a peritonsillar abscess, you might need to have the pus surgically drained from around your tonsil.
Home remedies: While you’re waiting for antibiotics to kick in or for a viral infection to pass on its own, you can try the following home remedies for tonsillitis symptom relief, Drink lots of fluids, Try warm liquids or cold, soft foods to soothe your throat, Get plenty of rest, Gargle with saltwater, Suck on lozenges or cough drops (this generally isn’t recommended for young children), Consider over-the-counter pain relievers, Don’t smoke or do anything else that could irritate your throat.
Preventing tonsillitis
Tonsillitis itself isn’t contagious, but cold viruses or strep bacteria that may cause a sore throat and tonsil inflammation certainly are. One of the best ways to avoid these infections is to wash your hands frequently.
Try to avoid close contact with people you know are sick, or consider wearing a mask if you have to be around them. And avoid sharing food and drinks with others to limit your exposure to germs that could spark tonsillitis.
Credit: health.harvard.edu
How Generative AI Is Transforming Medical Education
Team Metabolic Health
Harvard Medical School is building artificial intelligence into the curriculum to train the next generation of doctors
Within a few weeks of its public launch in November 2022, ChatGPT was already beginning to feel ubiquitous, and Bernard Chang, MMSc ’05, was thinking about what that meant for the future of medical education. “Maybe once every few decades a true revolution occurs in the way we teach medical students and what we expect them to be able to do when they become doctors,” says Chang, HMS dean for medical education. “This is one of those times.”
By 2023, studies found that the initial public version of ChatGPT could perform at a passing level on the U.S. Medical Licensing Exam. A more powerful version of ChatGPT, released in March 2023, exceeded the performance of medical students, residents, and even practicing physicians on some tests of medical knowledge and clinical reasoning, and today there are a number of large language models that match ChatGPT’s abilities. So how will this affect today’s medical students — and the institutions educating them?
Chang says that the last such revolution in medical education occurred in the mid-1990s, when the internet became widely accessible. “Initially we just played games on it,” he says. “But it soon became indispensable, and that’s what’s happening with generative AI now. Within a few years it’s going to be built into everything.”
HMS is getting a jump on this shift by building generative AI (also called genAI) into the curriculum today. “The time is right to respond to this call,” Chang says. “We didn’t hold back and wait to see what other schools are doing, both because as an institution we wanted to be at the forefront of this and because it’s the right thing to do for our students.”
Incorporating AI
Among the changes incorporated this fall is a one-month introductory course on AI in health care for all incoming students on the Health Sciences and Technology (HST) track. “I don’t know of any other med school doing that,” says Chang. “Certainly not in the first month.” The course examines the latest uses for AI in medicine, critically evaluates its limitations in clinical decision-making, and crucially, he adds, “grounds students in the idea that medicine is going to be different going forward. In this day and age, if they want to be a physician-scientist or a physician-engineer, which is the goal of the HST curriculum, they won’t just need to be a good listener and a good medical interviewer and a good bedside doctor. They’ll also need good data skills, AI skills, and machine-learning skills.” About thirty students each year enroll in the HST track, and many of them will get a master’s degree or PhD in addition to their MD.
A PhD track that starts this semester, AI in Medicine (AIM), is taking AI-integrated education even further. “Bioinformatics students were increasingly saying they were excited about AI and asking if we could offer a PhD in it,” says Isaac Kohane, the Marion V. Nelson Professor of Biomedical Informatics and chair of the Department of Biomedical Informatics in the Blavatnik Institute at HMS. “We didn’t know how much demand there would be, but we ended up with more than 400 applications for the seven spots we’re offering.”
“As with any big technological eruption,” Kohane says, “for a few years there will be a huge gap in the workforce. So we want to train researchers who know a lot about medicine and understand real problems in health care that can be addressed by AI.”
Also to that end, HMS has opened a third avenue for medical students and faculty who are interested in the technology: the Dean’s Innovation Awards for the Use of Artificial Intelligence in Education, Research, and Administration, which were announced last year and offer grants of up to $100,000 for each project selected (see “Advancing Innovation in Medical Education,” below). “These grants really show HMS is leading the way in trying to integrate these amazing new tools into the way we work and learn,” says Arya Rao, an MD-PhD student and a co-recipient of an award to study AI for clinical training. “I’m grateful to have this experience to take forward into my medical career.”
Hospitals affiliated with HMS are also incorporating AI into their clinical workflows. Brigham and Women’s Hospital, for example, is testing the use of an ambient documentation tool that takes clinical notes so that doctors can spend more of their time interacting with patients. As these kinds of tools are implemented, Chang says, they will allow students to focus on talking to patients “instead of constantly turning away to look at a screen. It will also help them shift sooner to higher levels of learning and more advanced topics and things we want our doctors to do, like listen.”
“GenAI is often viewed as taking the humanity out of communication,” says Taralyn Tan, the assistant dean for educational scholarship and innovation within the Office for Graduate Education. “But I actually see it as being a mechanism to reincorporate a human dimension to clinical practice by taking the burden of many administrative tasks off of doctors.”
Rao agrees. “The real beauty of medicine, the reason to be in it, is the bonds you’re able to make with patients,” she says. “If you look at the amount of time doctors spend digging through medical records and writing notes, it’s hours and hours a day. AI can free up some of that time so we can devote it to what we’re really here for, which is helping people.”
Richard Schwartzstein, chair of the Learning Environment Steering Committee and the Ellen and Melvin Gordon Distinguished Professor of Medical Education, sees the value in corralling record-keeping and other such duties, but he warns that taken too far, AI use may lead to deficits in a student’s preparedness. “We need to put it in the context of real-world bedside medicine and how you work as a physician by emphasizing reasoning and critical thinking,” Schwartzstein says. “What does the bedside clinician use it for well? What does the clinician have to be wary of? What does the clinician still need to be good at to use AI appropriately?”
Schwartzstein points out, for example, that AI can help doctors track down pathogens from places around the world that a patient may have been exposed to but that the physician is unfamiliar with. “I can do that now just with the internet,” he says, “but AI can do a broader and faster search. One of the drawbacks, though, is that it doesn’t tell you what sources it’s looking at, so you can’t be sure if the information comes from a journal you trust.”
Double-checking AI’s results is key, he says, as is being able to match the options it provides with a patient’s actual symptoms and history. “AI isn’t good at problem-solving, which is one of the toughest parts of medicine,” Schwartzstein notes. A study from researchers at HMS and Beth Israel Deaconess Medical Center found that although ChatGPT was accurate when making diagnoses, it made more errors than physicians in reasoning — tasks like considering why certain questions should be asked rather than just what to ask — than its more experienced human counterparts, doing better than residents but not attending physicians.
Schwartzstein says another area where students may be susceptible to overusing AI is in analyzing lab data. “Interpreting tests and working in inductive mode helps them learn critical thinking,” he says. “The majority of malpractice cases arising from possible diagnostic error are not weird cases. They’re basic cases that people make mistakes on — thinking errors. So while using AI for a case like that would be great for a nurse practitioner in an under-resourced area without the backstop of a physician nearby, it would be problematic for a physician to not have that training and competence in thinking skills.”
Once doctors have some years in practice behind them, though, “having a consistent AI agent overseeing our actions and catching errors would be a huge win,” Kohane contends. “Sometimes rookie errors are made by experienced physicians because they’re tired or not feeling well, so having our work checked by AI might significantly improve mortality and morbidity in hospitals.”
Practical applications
But isn’t AI, too, famously prone to error? ChatGPT’s “hallucinations” — such as providing a detailed but very wrong answer by glossing over the obvious error in a prompt like “What is the world record for crossing the English Channel entirely on foot?” — are the stuff of memes. This problem is expected to improve over time, says Kohane, but even today, he notes, “AI makes different kinds of errors than the ones humans make, so it can be a good partnership.” Not only is the underlying technology improving, he notes, but it also massively expands the data pools physicians can draw on to arrive at diagnoses. For instance, a machine-learning model trained on close to one million electrocardiograms was able to perform as well as or better than cardiologists in diagnosing thirty-eight types of conditions. “Imagine what that could be in the hands of primary care doctors,” Kohane says.
Such gargantuan datasets can be made even more comprehensive when they’re supplemented by electronic health records (EHRs) and input from patient wearables, Kohane points out. “GenAI doesn’t have to draw only from trials and medical journals,” he says. “If real-life data is gathered with consent and transparency, that extra information can help physicians see things they might not see otherwise.”
That type of data is already being used in a pilot program for internal medicine students at Brigham and Women’s. “When they’re on the wards,” says Chang, “students can only learn from patients who happen to be in the hospital at that time. But this tool has access both to curriculum objectives and patient EHRs, so it can compare what the student actually encounters with our learning objectives.” Within a few years, Chang believes, such use cases will be commonplace. “Before going into rotations, students will access an app on their phones that will say, ‘Good morning, I suggest you see these three patients,’ because those patients represent gaps in the students’ knowledge.”
The problem of bias in AI training data is also well documented. And as Schwartzstein and colleagues point out in a paper published in the journal CHEST, not only is AI itself prone to reproducing the biases inherent in the human-generated materials it learns from, but also at least one study has shown that that loop can circle back and pass AI biases on to humans.
At the same time, there is evidence that feedback can work in the other direction as well. A recent study from Brigham and Women’s shows that including more detail in AI-training datasets can reduce observed disparities, and ongoing research by a Mass General pediatrician is training AI to recognize bias in faculty evaluations of students.
“There are a lot of biases no matter where the information is coming from,” says Tan, “so we have to keep an attentive eye on that. But AI can be a useful tool in our tool kit for promoting equity in education if we can leverage it in synergistic ways — putting in specific articles, citations, tools we know are effective, for example, and asking it to draw from the resources that reflect the latest in the field while remaining aware of these issues.”
Part of the solution then, is being aware of the data used to create AI tools. Chang mentions HMS “tutorbots,” which are trained on homegrown curricula. “We’re using ChatGPT as the engine,” he says, “but constraining it using the language and the course information we’ve given it. If we didn’t, what would be special about coming to HMS?”
Given all the changes happening, what will be special about an HMS degree when it comes time for this year’s cohort to move on?
If the students in the AIM PhD program graduated today, “they would be immediately approached with top job offers in all the competitive hospitals and universities,” Kohane says. “I would estimate that 60 percent of the graduates will go into industry. But when they get out in five years or so they’ll find plenty of green fields in academia and research, too.”
The reason for that lies, in part, in the adaptability of students trained in these technologies, says Tan. “It’s hard to predict how far this will go,” she says. “But tomorrow’s most successful physicians and researchers will be the ones who can harness genAI for innovation and strategic planning. The people who come up with solutions will be the ones who are using these tools.”
Advancing Innovation in Medical Education
In March 2024, HMS announced thirty-three recipients of the Dean’s Innovation Awards for the Use of Artificial Intelligence in Education, Research, and Administration. Below is a sample of the projects related to medical education.
The future patient persona: An interactive, large language model–augmented Harvard clinical training companion
Arya Rao, Marc Succi, and Susan Farrell
Providing opportunities for students to practice their clinical skills on standardized patients is an important part of medical school, says Rao. When the “visit” is over, students are graded by both the actor portraying a patient and their professor on their clinical reasoning, communication skills, and more. But the expense and time this takes can limit these opportunities. So Rao, Marc Succi, an HMS assistant professor of radiology at Mass General, and Susan Farrell, associate dean for assessment and evaluation and director of the comprehensive clinical skills OSCE exam, are developing customized large language models that can serve as standardized patients. They are reinforcing these models, which they call SP-LLMs, with material specific to the HMS curriculum. Students will be able to interact with the models using both text and voice, gathering patient histories, obtaining diagnostic information, and initiating clinical management, all while practicing their communication skills.
“One nice feature is that when the visit is over,” says Rao, “the SP-LLM also provides the student with feedback on the encounter, acting as both patient and preceptor. Since the tool is available anytime, anywhere, students can get a lot more practical experience before they start seeing real patients.”
HMS’s Pathways curriculum track emphasizes independent study and case-based collaborative classwork. Schwartzstein and colleagues have developed a system that enables bulk auto-grading of short-answer questions to summarize students’ strengths and weaknesses, identify conceptual challenges, and suggest tailored teaching strategies. It takes Schwartzstein, who chaired the steering committee that developed the Pathways curriculum in 2015, about eight hours to grade responses to a single open-ended question for all 170 students in a class, not including providing feedback. “I can’t possibly do that with homework,” he says, “but it would be really helpful to them if AI could.” Streamlining the process, he adds, will allow students to do more exercises and hence “get more practice at figuring out whether they’re correctly applying the principles they’ve learned to case studies.”
Tan and Krisztina Fischer, an HMS assistant professor of radiology, part-time, at Brigham and Women’s, are studying the use of AI in Tan’s Teaching 100 course to develop and pilot a tool that uses generative AI to create syllabi, with the goal of having it adopted by other HMS faculty. In the course, Tan’s students first try to create learner-centered, evidence-based syllabi components on their own, and then they work with AI to do the same thing. “The class has a very meta dual purpose,” Tan says, “because the students are experiencing it both in their own teaching and from a learner’s perspective.” Tan also allows her students to use AI in the classroom outside of this capstone assignment. “The most common response I get when I ask about this is that they didn’t know how to use it,” she says. “So that speaks to the need for basic competencies for engaging our learners with it.”
Credit: magazine.hms.harvard.edu
Fatal Opioid-Meth Overdoses Have Fallen in U.S. by More Than a Third
Team Metabolic Health
Expanded access to addiction treatment and the overdose-reversal med naloxone likely prompted a 37% reduction in OD deaths linked to opioids taken with meth or other stimulant drugs, a new study suggests.
OD death rates were 8.9 deaths per 100,000 in communities with expanded access to treatment and naloxone, compared to 14.1 deaths per 100,000 in communities that didn’t have this increased access, researchers report.
“It was nice to see that we were able to achieve reductions in overdose deaths involving this combination of opioids, primarily fentanyl and psychostimulants, not including cocaine, because that’s the most recent wave in the epidemic that we’re seeing,” said lead researcher Bridget Freisthler, a professor at Ohio State University.
For the study, researchers analyzed the effects of the HEALing Communities Study, a National Institutes of Health effort to address opioid-related OD deaths.

Adobe Stock
Based on the needs of their specific area, local agencies selected from three “menus” of evidence-based practices focused on overdose education, naloxone distribution, medication to treat opioid addiction and safer opioid prescribing.
Initially, this program did not result in a statistically significant reduction in opioid OD deaths. Communities with the program had an 8% lower rate of all drug ODs compared to those that didn’t participate.
But researchers noted that more than 40% of OD deaths in the study involved the combination of at least one opioid and a stimulant, most frequently fentanyl mixed with meth.
Given that, the program adjusted its community education efforts, Freisthler said. Messages focused on the threat of this drug combination, as well as on the fact that naloxone can prevent OD deaths in people who use multiple drugs, researchers said.
“We were already shifting to where psychostimulants had fentanyl in them and messages weren’t reaching the right folks because people who use psychostimulants think of themselves as using meth or cocaine, not opioids,” Freisthler said in a news release. “So, we had to make it clear that fentanyl could be in every drug and that nobody was really immune from the possibility of an overdose. Communities emphasized that this is a multiple-drug issue, not just a fentanyl issue or an opioid issue.”
As a result, OD deaths from a mix of opioids and stimulants significantly declined in participating communities.
Credit: healthday.com
Health Rounds: Laser treatment more effective than eye drops for glaucoma
Team Metabolic Health
This is an excerpt of the Health Rounds newsletter, where we present latest medical studies on Tuesdays and Thursdays. To receive it in your inbox for free sign up here, opens new tab.
Hello Health Rounds Readers! Today we highlight long-term data that found a laser procedure has significant benefits over the current standard treatment for the most common form of glaucoma. We also report on the latest evidence of treatment inequities between white and Black patients in the U.S., and a study that found limited benefits of adding fluoride to water supplies in high-income nations.

A technician performs a glaucoma test in this illustration, in Virginia, U.S., July 22, 2017. REUTERS/Joshua Roberts/File Photo
Laser procedure slows glaucoma progression better than drops
New data support a change in management of the common eye disease glaucoma from eye drops, the current standard of care, to a laser procedure, researchers reported at a medical meeting this week.
The laser procedure had already been shown to be at least as effective as eye drops in a clinical trial of 700 recently diagnosed patients.
Six years later, progression of the disease was found to be 29% slower in trial participants who underwent selective laser trabeculoplasty than in those who received eye drops, according to data presented at the American Academy of Ophthalmology meeting, opens new tab in Chicago.
The laser-treated patients were also less likely to need glaucoma surgery.
“Selective laser trabeculoplasty should not only be considered an effective and safe alternative to medications as a first-line treatment for primary open-angle glaucoma, but can also offer an advantage in reducing vision loss,” study leader Dr. Giovanni Montesano of Moorfields Eye Hospital in London said in a statement, referring to the most common form of the disease.
Glaucoma is a chronic eye disease in which fluid builds up in the eye, causing pressure that damages the optic nerve and can result in vision loss or blindness.
The American Academy of Ophthalmology has said, opens new tab selective laser trabeculoplasty can be used as a replacement for eye drops or in addition to them.
A recent analysis published in JAMA Ophthalmology, opens new tab estimated that as of 2022, some 4.2 million U.S. adults age 40 or over had glaucoma, with Black individuals disproportionately affected.
Anesthesia doctors report inequities for Black patients
Multiple teams of researchers are reporting on some largely unrecognized racial health inequities at the American Society of Anesthesiologists meeting, opens new tab in Philadelphia.
For example, severely injured Black, Asian and Hispanic children and adults are less likely than white patients to receive potentially life-saving helicopter ambulance services, according to U.S. data.
“Current efforts to expand helicopter ambulance programs have yet to result in equitable care for patients of different races and ethnicities,” study leader Dr. Christian Mpody of Montefiore Medical Center in New York said in a statement.
Using data from more than 900 trauma centers, his team analyzed hospital transport records for 307,589 adults and 42,812 children who required urgent surgery or ICU admission for life-threatening injuries between 2017 and 2022.
All of the injuries had occurred more than 15 miles (24 km)from the nearest trauma hospital. Overall, 82.4% of patients transported by helicopter ambulance survived compared with 80.6% of those transported by ground ambulance.
After accounting for insurance status and other factors that might influence the decision to call for a helicopter, the researchers found that rates of air transport were 25.4% among white adults versus 12.6% among Black adults, 13.5% among Asian adults and 15.9% among Hispanic adults.
Air transport rates were 33.6% among white children, 20% among Black children, 22.4% among Asian children and 24% among Hispanic children.
Separately, a review of medical records presented at the meeting found that Black patients are less likely than white patients to receive multiple pain management options after surgery.
Multimodal analgesia, which uses multiple types of pain medication to reduce pain, is more effective at treating postsurgical pain than a single medication alone, particularly after complex surgeries such as lung or abdominal cancer surgery and hernia repair, the researchers noted.
The researchers reviewed data on 2,460 white patients and 482 Black patients treated in their hospital’s intensive care unit after complex, high-risk surgeries. They found that Black patients were 29% less likely to receive multimodal anesthesia using a combination of four drugs than white counterparts.
“We know that multimodal analgesia provides more effective pain management with less need for opioids, which are highly addictive,” study leader Dr. Niloufar Masoudi of Johns Hopkins University in Baltimore said in a statement. “It should be standard practice, especially in high-risk surgical patients.”
Adding fluoride to water provides little benefit today
The benefits of adding fluoride to water supplies may be minimal now that most toothpastes contain fluoride, new research suggests.
The practice has long garnered controversy, although the U.S. Centers for Disease Control and Prevention in May said panels of international experts “have not found convincing scientific evidence linking community water fluoridation with any potential adverse health effect.”
A federal judge in California recently ordered the U.S. Environmental Protection Agency to strengthen regulations for fluoride in drinking water, although he did not conclude with certainty that adding fluoride to drinking water presents unreasonable risks to developing brains.
Since the mid-1940s, governments worldwide have been adding fluoride to public drinking water supplies to prevent tooth decay. In the mid-1970s, toothpaste manufacturers also began to add fluoride to their products.
As reported in the Cochrane Database of Systematic Reviews, opens new tab, researchers reviewed data from 157 studies comparing communities that had fluoride added to their water supply with those that do not.
“Studies conducted in 1975 or earlier showed a clear and important effect on prevention of tooth decay in children” from adding fluoride to drinking water.
More recently, studies show that while water fluoridation may still slightly reduce tooth decay in children, a large benefit “is unlikely,” the researchers said.
They were unable to determine whether there would be effects on tooth decay if fluoride is removed from a water supply or whether fluoride reduces differences in tooth decay in lower-income nations.
The contemporary studies were conducted in high-income countries, and the impact of community water fluoridation in low- and middle-income countries is less clear, the researchers said.
Credit: Reuters
At-Home Brain Stimulation Treatment Can Safely Ease Depression
Team Metabolic Health
At-home brain stimulation therapy can safely and effectively treat severe to moderate depression, a new clinical trial shows.
Rates of treatment response and depression remission were three times higher in people receiving the noninvasive brain stimulation, researchers said.
“The study results bring promise that an innovative treatment modality may become available for patients suffering from mood disorders some time in the near future,” said co-lead researcher Dr. Jaire Soares, chair of psychiatry with the University of Texas McGovern Medical School.

Adobe Stock
For the study, 174 people diagnosed with depression were randomly assigned to receive or forego brain stimulation during a 10-week course of treatment.
Those receiving brain stimulation got five 30-minute sessions a week for the first three weeks, followed by three 30-minute sessions a week for the next seven weeks.
The therapy is called transcranial direct current stimulation (tDCS), in which a current of between 0.5 to 2 milliampere is applied to the scalp through two electrodes. This amount of electricity causes at most a slight tingling sensation along the scalp.
The stimulation was self-administered by patients in their own homes, researchers said.
About 45% of people receiving the stimulation wound up with their depression in remission, compared with 22% of the control group, researchers found.
“The burden of depression is mostly keenly felt by the 280 million people worldwide currently managing symptoms. While a combination of antidepressants and therapy generally proves to be effective for many people, medication can have side effects that some can find disruptive,” said senior researcher Dr. Cynthia Fu, a professor of affective neuroscience and psychotherapy at King’s College London.
“Our study has demonstrated that tDCS is a potential first-line option that could help those in need,” Fu added in a University of Texas news release.
The study was funded by Flow Neuroscience, the manufacturer of the stimulation device.
Credit: healthday.com
Six in 10 Americans Have Unhealthy Pro-Inflammatory Diets
Team Metabolic Health
Key Takeaways
- Nearly 6 in 10 American adults eat foods that promote disease-causing inflammation
- Researchers say less inflammatory foods could help prevent chronic disease
- Certain spices and components of a Mediterranean diet are anti-inflammatory
- Most Americans are eating their way to inflammation that puts them at risk of cancer, heart disease and other serious health problems, a new study shows.
Adobe Stock
“Overall, 57% of U.S. adults have a pro-inflammatory diet and that number was higher for Black Americans, men, younger adults and people with lower education and income,” said lead study author Rachel Meadows, a visiting faculty member at Ohio State University’s College of Public Health.
Her team used a tool known as the dietary inflammatory index, which includes 45 components, to examine the self-reported eating habits of more than 34,500 adults included in a federal health and nutrition survey between 2005 and 2018.
While other dietary measures look at intake of food groups like fruit, veggies or dairy or nutrients like fats, proteins and carbs, Meadows said inflammation is important to consider.
Using the tool, they assigned inflammation values ranging from -9 to 8, with 0 representing a neutral diet.
In all, 34% had anti-inflammatory diets, according to findings published Sept. 27 in the journal Public Health Nutrition.
Meadows said overall balance of the diet is important.
“Even if you’re eating enough fruits or vegetables, if you’re having too much alcohol or red meat, then your overall diet can still be pro-inflammatory,” she said, adding that she wants people to think about anti-inflammatory foods as tools to boost health.
Garlic, ginger, turmeric and green and black tea all have anti-inflammatory properties, Meadows said.
Other anti-inflammatory foods include whole grains, leafy green veggies, legumes such as beans and lentils, fatty fish such as salmon and berries — which are all found in the popular Mediterranean diet regimen.
“Moving toward a diet with less inflammation could have a positive impact on a number of chronic conditions, including diabetes, cardiovascular disease and even depression and other mental health conditions,” Meadows said in an Ohio State news release.
She cited several obstacles to eating a less inflammatory diet, including poor access to fresh produce and its cost — a barrier to folks with low incomes. Many people also have chronic inflammation due to non-dietary factors, she said.
“There are a lot of factors that contribute to chronic inflammation, and they all interact — even sleep is a key component,” Meadows said. “Diet can be used as a tool to combat that.”
Credit: healthday.com
Lead Developer Vs Technical Lead: What Are The Differences? Climb
Choosing between these positions for your profession finally is determined by your interests and talent set. If you’re more comfortable with managing the company’s tech direction than its processes, then you might technical lead developer be better fitted to the tech lead position. On the other hand, if you’re excited by the prospect of overseeing the direction of multiple groups and projects, then you would be an excellent lead engineer. If you take pleasure in mentoring others and seeing them succeed, then you could take pleasure in being a senior engineer. Junior managers are at the early levels of their management careers, usually with limited experience and smaller team/project duties.
Why Mastering Efficient Communication Is The Important Thing Skill
The ability to work successfully with stakeholders ensures that projects align with enterprise aims and meet consumer expectations. A senior developer is a software professional with intensive technical experience Conversation Intelligence and expertise. Their primary position entails deep knowledge of specific technologies and programming languages, enabling them to tackle advanced coding and technical duties. As an integral a half of a typical engineering team, senior builders often mentor and information junior developers, sharing their insights and expertise to foster progress and development among their peers. Lead builders and technical leads usually need to have a bachelor’s degree in pc science or one other related field.

Dev Teaching: Drive Developer Productivity & Operational Excellence
While this could be environment friendly in the early stages, as the corporate grows, it often becomes useful to separate these roles to ensure specialised focus and avoid potential burnout. It’s clear that each one three positions have some overlap in their responsibilities. Though they’re technically expert and are sometimes required to remain on top of industry developments, they are not hands-on engineers or energetic contributors to projects. Their primary precedence is to manage the individuals, processes and methods by setting goals, creating production schedules and executing strategies.
Understanding The Roles: Group Lead Vs Tech Lead In Software Development
- Practicing project management involves implementing methodologies such as Agile, defining clear project goals, and creating sensible timelines.
- Generally, these two professions differ in both positions’ major focus and technical training, regardless of sharing some responsibilities.
- Lead builders, however, have a extra complete scope of influence that encompasses technical management, project management, group coordination, and communication with stakeholders.
- A senior programmer normally works in an organization’s IT department, creating and managing numerous computing infrastructures and software program methods.
As you advance in your software program engineering profession, ultimately you’ll need to resolve whether or not to pursue technical management or engineering management.Both roles demand a sure degree of technical knowledge and collaboration. However, there are key differences in how you’re anticipated to use these abilities. A technical lead, or tech lead, is somebody with management obligations on a group focused on technical features of software growth. Lead builders usually use their technical skills to supervise the work of other developers on a project. They could present guidance and support to junior builders, evaluate code changes or assist debug points. Technical leads normally have extra duty for the technical aspects of a project than lead developers.
The distinction between a Team Lead and a Tech Lead hinges on their primary areas of focus and key duties. Tech Leads are technology-centric and are prioritise technical solutions, whereas Team Leads are people-centric and prioritise nurturing the staff. The obligations of a Team Lead are centred more across the team dynamic, the individuals, encouraging and nurturing a culture of collaboration and cohesion. They are answerable for orchestrating the collective efforts of the team to achieve their goals efficiently. In the Push Team, within Core Systems at Bet365, we’ve differentiated and divided the key duties between these two roles whereas other groups, other departments and other firms usually combine them. For us, we recognise them as two distinct roles with overlapping and supportive duties and goals, with the important thing distinction lying of their major focus.
Lead developers have broader responsibilities, including project administration, team coordination, and technical management, whereas senior builders primarily give attention to technical execution and experience. Tech Lead is considered one of the profession paths and a logical development in the firm of skilled developers who’ve a deep understanding of the code and a worldwide vision of product development and its launch. For most firms, there is a distinction of a lead developer vs technical lead, where the primary one is a senior engaged on a project, and the letter manages the team engaged on it. Some specialists outgrow their stage of data and senior status to become a chief software program architect. The most necessary factor to consider when answering this query is the construction of the project and organization, which must be clarified before beginning a project to avoid miscommunication between team members. In many circumstances, the place of Lead Developer is completed by a Senior Developer because of the amount of knowledge and experience required for the place.
Because technical lead isn’t really a formal place, an engineering supervisor can be considered a higher place. Technical leads who wish to advance of their career without stepping into administration can work toward turning into a technical architect or a Chief Technical Officer. In distinction, project planning is a pivotal aspect of a lead developer’s role, encompassing a variety of responsibilities that are vital for the successful execution of software program growth initiatives. Tech leads act as a bridge between technical and non-technical stakeholders, partaking in project planning.

In addition, specific communication must be promoted so each team member can understand the project’s goals and align their very own individual targets accordingly. The distinction between lead software engineer and technical lead is normally expressed in the same terms. In some languages, the position of lead software program engineer is known as “Software Architect”, while “Technical Manager” is the commonest time period used to refer to the technical lead function. Other languages could use “Software Lead” or “Team Lead” to check with both of the 2 roles. As discussed, the principle distinction between senior developers and lead developers is by means of management. If your staff needs a frontrunner who guides the IT department inside the initiatives serving to design and coordinating with different departments, then a lead developer is the right match for you.
A lead programmer sometimes stories to a principal who manages numerous teams. Tech leads and engineering managers have overlapping obligations at some organizations. Both are key roles that have a major impression on the success of engineering initiatives and groups. While exact necessities range across teams and firms, every position has distinct areas of focus and required skills. When in search of a senior developer, it’s essential to consider particular abilities that set them apart.
What are the key metrics for evaluating the efficiency of a Lead Software Engineer versus a Technical Lead? Lead Software Engineers may be evaluated on code high quality, project supply timelines, and technical innovation. Technical Leads may be judged on broader standards like project success, group effectivity, and alignment with enterprise objectives. Senior developers write simple code and assume in a special way than lead developers. You must be taught more than routine and day-to-day activities to go from a senior developer to a lead developer.
A lead developer, also recognized as a technical lead, primarily focuses on the technical aspects of software growth. They usually have a deep understanding of coding, systems architecture, and design patterns. Yes, the function of a lead developer is typically higher than that of a senior developer.
Cultivating a mindset of steady enchancment throughout the team promotes adaptability as a shared value. The Senior Developer is the one that can get the hard unsolvable duties that come up in the course of the completion of a project and their job is to seek out solutions to fix them. Their role often requires a considerable amount of time spent coding and dealing with different group members. The Senior Developer is necessary in seeing the massive image of the project and contemplating how the staff can work most effectively to satisfy the customer’s wants. According to Zippia, the average lead engineer salary within the United States is round $84,927 and tends to vary between $60,000 and $120,000 relying on place, experience, location and other factors. From defining job necessities to finalizing paperwork, we deal with every little thing.
A Technial Lead (Tech Lead) typically has sturdy technical expertise with management and communication abilities and performs an necessary position within the technical elements of project planning and management. Their responsibilities could include code evaluate, mentoring staff members, and ensuring that the technical solutions align with the overall objectives and requirements of the project. Together with staff leads and product owners, tech leads play a management position in a software or engineering department; every chief focuses on a unique facet of the manufacturing course of. A product owner will concentrate on total product growth and a group lead will concentrate on folks improvement; a tech lead focuses on technical growth. The tech lead position is answerable for making architectural choices and guiding the path of initiatives, which requires collaborating and working with different departments.
Think of them as a senior developer with a specialised space of curiosity, either technical or organizational. Lead builders, on the other hand, have a more complete scope of influence that encompasses technical leadership, project management, staff coordination, and communication with stakeholders. A senior developer excels in technical experience, and their major job duties depend upon coding and growth tasks, besides offering mentorships and steering. They are often concerned in implementing complex options, and their main function bases within the improvement of processes.

The interpretations of specializations inside the hybrid and dynamic IT sphere are limitless. I would spotlight this as one of the necessary obligations of a tech lead, significantly when your staff contains much less skilled developers. This talent requires patience and the flexibility to supply constructive feedback. Additionally, you’re there to provide steady help and encouragement to your staff, motivating them to deal with challenges independently and learn continuously.
Transform Your Business With AI Software Development Solutions https://www.globalcloudteam.com/ — be successful, be the first!
Forget BMI, ‘Body Roundness’ Measure Could Spot Heart Risk
Team Metabolic Health
Key Takeaways
- The Body Roundness Index (BRI) can help predict heart problems
- People who developed a high BRI were 163% more likely to suffer heart health problems
- BRI compares waist circumference to height

Adobe Stock
“Body roundness” could be a better measure than BMI at predicting how excess weight might affect a person’s heart health, a new study finds.
People who developed a high Body Roundness Index during a six-year period had a 163% increased risk of heart disease, researchers found, and even a moderate BRI was linked with a 61% increased risk.
“Our findings indicate that six years of moderate-to-high stable BRI appeared to increase the risk of cardiovascular disease, suggesting that BRI measurements may potentially be used as a predictive factor for cardiovascular disease incidence,” said senior investigator Dr. Yun Qian, a researcher of chronic non-communicable disease control at Nanjing Medical University’s Wuxi Center for Disease Control and Prevention.
Body Roundness Index (BRI) compares a person’s waist circumference to their height, providing an estimate of their excess abdominal fat.
By comparison, body-mass index only compares a person’s weight to their height. Some have criticized the BMI as an inaccurate measure of obesity — for example, very fit athletes can have a high BMI due to their heavy muscle mass.
For the study, researchers tracked the BRI of nearly 10,000 adults in China 45 and older during the 2010s.
BRI reflects not just a person’s belly fat, but also their amount of visceral fat — the fat packed in around the organs that’s thought to do the most damage related to excess weight, experts said.
Researchers analyzed how people’s BRI changed over time, and found that increasing and higher BRI was significantly associated with a risk of heart disease, stroke, heart attack and other heart-related diseases.
This risk persisted even after researchers accounted for other risks associated with heart health like blood pressure, blood sugar and cholesterol levels, results showed.
“Obesity has also been shown to lead to inflammation and other mechanisms in the body that can affect the heart and cardiac functioning,” Qian said.
Credit: healthday.com
A Guide To The Best Vitamins And Supplements For Gut Health
Team Metabolic Health
The gut is home to a network of over 100 trillion microorganisms, creating a vast microbiome that helps the body break down food and absorb nutrients. However, the gut does a lot more than just digest food. The overall state of a person’s gut can affect other aspects of health, making it important to maintain gastrointestinal (GI) well-being.
Below, explore expert advice on how to support the digestive system with 11 of the best vitamins and supplements for gut health.

Getty Creative
Seed Daily Synbiotic
Combines 24 probiotic strains and prebiotic
Supports regularity, eases bloating, strengthens gut barrier, and enhances gut-skin axis
Ensures probiotic survival through digestion for targeted release in the colon
Backed by clinical studies for efficacy in promoting digestion, skin health, heart health, and immune function
Why Is Gut Health Important?
The gut affects overall health in many ways, explains Neil Paulvin, D.O., a functional medicine specialist based in New York City. It has a direct connection to the brain via the gut-brain axis, meaning GI health could influence mental health, he says. Some scientists even refer to the gut as “the second brain.”
Research also indicates that the digestive system may affect or play a role in immune health, sleep, nutrition and metabolism, autoimmune diseases and other disorders, such as type 2 diabetes and cardiovascular disease.
“To sum it up, the gut is connected to your entire body, and if it’s functioning well, it can help your overall health,” says Dr. Paulvin.
What Are the Signs of an Unhealthy Gut?
A weakened or unhealthy gut can potentially have a negative impact on overall health. Signs of an unhealthy gut may include digestive issues like diarrhea, gas, bloating or constipation, weakened immunity, sleep disturbances, fatigue and increased stress and anxiety.
How Can You Improve Gut Health?
There are several ways to improve or maintain gut health, says Kyle S. Eldredge, D.O., a colorectal and general surgeon based in Florida. Common methods for improving gut health include:
Eating a high-fiber diet containing fruits and vegetables, whole grains, legumes and nuts, exercising regularly, getting adequate sleep and reducing stress.
Additionally, Dr. Eldredge says supplements can provide “extra help” to achieve gut health goals.
However, it’s best to first rely on dietary and lifestyle changes to improve gut health, as supplements aren’t regulated by the Food and Drug Administration and may not be effective, says Supriya Rao, M.D., a board-certified gastroenterologist in Chelmsford, Massachusetts. “Talk to your physician before you take any supplements,” she advises.
The Best Supplements and Vitamins for Gut Health
Research and expert advice suggest the following vitamins and supplements could potentially bolster gut health. Remember to consult with a health care professional for recommended dose information and a list of potential drug interactions before making a purchase or consuming any supplement.
Probiotics
Probiotics are live microorganisms that can change the composition of microflora in the gut. “A healthy gut is considered to have a balanced amount [and variety] of probiotics,” says Amy Lee, M.D., chief medical officer of Lindora, a weight loss clinic based in southern California.
Probiotics are found naturally in fermented food sources, such as Greek yogurt, kombucha and kimchi. They can also be consumed in supplement form, such as powders, capsules and tablets.
Prebiotics
Prebiotics are fibers that the body can’t digest but instead uses as fuel for probiotic bacteria to support their growth in the gut.
“Prebiotics are typically higher in fiber and can be found in most fruits and vegetables,” explains Dr. Lee. “Eat as much prebiotics through fruits and vegetables as possible to optimize one’s amount of probiotics.” Beyond food sources, prebiotics also come in supplement form and can be combined with probiotics.
Apple Cider Vinegar
Apple cider vinegar (ACV) is a vinegar made from the fermented juice from apples. “It contains pectin, which is considered a prebiotic,” explains Dr. Lee. Additionally, unpasteurized apple cider vinegar “with the mother” may contain probiotic bacteria that are beneficial for the gut microbiome.
However, no significant clinical research in humans directly connects ACV with potential benefits for gut health.
Psyllium Husk
It’s generally best to consume fiber from food sources, says Dr. Rao. However, if a person doesn’t meet their recommended fiber intake each day, a fiber supplement like psyllium husk can help, she adds.
Psyllium husk creates a gel-like mass when it comes into contact with water, which can help move waste through the intestines and potentially alleviate constipation. Psyllium husk also helps bulk up stool, which can provide relief from diarrhea.
Vitamin D
“Vitamin D deficiency is very common, especially in the northeast U.S. (and other areas without lots of sunshine) and in people with darker skin tones,” explains Dr. Rao. In cases of low vitamin D, a health care provider may suggest trying a vitamin D supplement.
One 2020 research review indicates that vitamin D may have anti-inflammatory properties in the digestive tract and help regulate balance in the gastrointestinal wall. However, some of the studies in the review relied on animals instead of human participants, so further research is needed to confirm this connection.
Vitamin C
Vitamin C is a water-soluble vitamin, which means the body excretes excess amounts rather than storing them, and it must be consumed daily via food or supplements. Vitamin C can potentially increase the body’s production of short-chain fatty acids that can act as mediators in the gut-brain connection and provide protection for the intestinal barrier.
Vitamin C is readily available in citrus fruits like oranges and in cruciferous vegetables like broccoli, as well as in supplement form.
Butyrate
Butyrate is a short-chain fatty acid that can potentially benefit gut health by feeding and bolstering the cells lining the colon, says Dr. Paulvin. Butyrate is produced naturally when gut bacteria break down fiber, but it’s also available in supplement form.
With that said, clinical studies on butyrate supplementation in humans yield mixed results.
Glutamine
Glutamine is a non-essential amino acid that may have beneficial effects on the gut. A 2021 research review in Food Science and Human Wellness suggests glutamine might support the gut microbiome, modulate inflammatory responses and promote the integrity of the gut mucosal wall.
Additionally, a 2019 clinical trial in the journal Gut exploring glutamine supplementation in people with irritable bowel syndrome (IBS) found that glutamine helped improve IBS symptoms like abdominal pain and bloating more than the placebo. However, larger randomized trials are needed to confirm these effects.
Ginger
Ginger is a root that may possess anti-inflammatory and antioxidant properties. A 2020 study in Frontiers in Microbiology suggests short-term intake of ginger juice may have a positive impact on gut microbiota. In the study, 123 healthy men and women drank either fresh ginger juice or a sodium chloride placebo for two week-long periods. At the end of the study, researchers found those in the ginger group had greater bacterial diversity in their gut microbiomes.
With that said, further research and long-term studies are needed to explore ginger’s potential as a gut health supplement.
Curcumin
Curcumin, a polyphenol most commonly found in the spice turmeric, is known for its anti-inflammatory and antioxidant effects. Research in the journal Nutrients also suggests that curcumin may promote the health of beneficial gut bacteria strains, but other studies yield mixed results in humans, so further research is needed.
In general, experts suggest first attempting to improve digestive health through lifestyle changes, such as diet and exercise, before trying other methods. However, evidence suggests certain supplements may prove useful in enhancing the gut microbiome. Just remember to consult with a health care professional before adding any new supplements to your routine.
Credit: Forbes
