Ozempic underworld: Inside the black market of obesity drugs
Team Metabolic Health
BOULDER, COLO. — Not far from the majestic Rocky Mountains is an ordinary suburban neighborhood, a tree-lined street and a modest light gray home.
It’s not the kind of place you’d imagine an investigation into black market Ozempic would lead. But it did.
A CNBC investigation into counterfeit weight loss drugs revealed an international illegal marketplace where criminals either brazenly alter the drugs or ship the real product from overseas — what’s known as drug diversion and against federal law.
The operations mainly involve phony or illegal versions of Novo Nordisk’s diabetes drug Ozempic and its obesity drug Wegovy as well as Eli Lilly’s Mounjaro and Zepbound. All four drugs are in a class of wildly popular weight loss drugs known as GLP-1s. The skyrocketing demand for the treatments has led to criminal schemes attempting to capitalize on the surge.
CNBC bought a drug marketed as Ozempic from a company called Laver Beauty, which on its website and corporate documents listed its address on that quiet residential street in Boulder. The drug cost $219 for a month’s supply, a fraction of the list price of $968 for a month’s supply of Ozempic in the U.S.

The owners of the home in Boulder say they have no connection to the company — though they’ve received mail and a 1099 IRS tax form addressed to Laver Beauty.
The drug CNBC purchased was shipped via DHL from an office building in Shijiazhuang, China, about a four-hour drive from Beijing. The package that arrived at CNBC headquarters in Englewood Cliffs, New Jersey, was a plain cardboard box with no refrigeration except for two melted ice packs. Ozempic is supposed to be stored refrigerated. The drug packaging, which appeared authentic, featured Chinese writing and the Novo Nordisk logo.
In an email, Novo Nordisk said the drug appeared to be “diverted legitimate product that was produced for, and distributed to, the Chinese market during late ’23 and early ’24. Therefore, it would be unauthorized/unapproved for the US market.”
The company added that it “cannot confirm the sterility, which may present an increased risk of infection for patients who use the counterfeit product.”
Law enforcement sources told CNBC that the Ozempic received from China is part of a larger ongoing federal investigation into Ozempic packages being shipped to the U.S.
Laver Beauty did not respond to CNBC’s request for comment, but a person who identified himself as a company representative told CNBC in a WhatsApp chat, “All our products are genuine. We don’t sell fake ones.” The person acknowledged that the product CNBC purchased was intended for the Chinese market.
The representative also messaged that the Boulder address “is the previous address of our U.S. warehouse.” A day after CNBC inquired about the Boulder address, it was removed from the company’s website.
Counterfeit medication
The Ozempic that CNBC purchased is considered an illegally diverted drug. A separate but related growing problem is the rise of counterfeit drugs — fake products purporting to be the real thing.
In the United Kingdom, authorities last year seized hundreds of counterfeit Ozempic pens — insulin pens that had been relabeled as Ozempic.
“We saw that the demand increased and quite often as it happens in these situations, criminals try and fill a gap where the supply and demand aren’t balanced for a particular product, and we started seeing real counterfeit versions of the Ozempic product on the market,” said Andy Morling, deputy director of criminal enforcement for the U.K.’s Medicines and Healthcare Products Regulatory Agency.
Morling spoke to CNBC from a warehouse outside London where the counterfeits are stored. A total of 869 Ozempic counterfeit pens were seized in 2023.
Counterfeit weight loss drugs have serious health risks, according to the pharmaceutical companies and federal officials. In some cases they could be fatal to someone using them.
Eli Lilly, the maker of Mounjaro and Zepbound, said it is actively fighting the counterfeits.
“We have a very elaborate and rigorous system to test medicines before they’re allowed to be used in patients. But unfortunately [counterfeits] don’t go through that system at all,” said Dr. Daniel Skovronsky, Eli Lilly’s chief scientific officer and president of Lilly Research Labs.
He showed CNBC a sophisticated fake that was labeled as Mounjaro but that contained a different medication entirely — one for Type 2 diabetes that doesn’t cause weight loss.
“It looks to all the world like Mounjaro, comes in a box that’s labeled as Mounjaro,” he said. “And it has pens that are labeled as Mounjaro. But it’s not Mounjaro at all.”
Counterfeiters are already trying to cash in on a weight loss drug that the company hasn’t even put on the market yet: retatrutide. CNBC found it’s being sold online.
“We’re testing it in Phase 3 clinical trials today. We don’t know yet, but I hope to get those results next year and we’ll find out,” Skovronksy said.
Asked about sites selling what they claim is retatrutide, Skovronksy said, “Yeah, that’s crazy … Even the real retatrutide is not ready for patient use outside of clinical trials.”
Port seizures rising
Finding fake or diverted Ozempic and other obesity drugs is common at the sprawling international mail facility located on the grounds of John F. Kennedy International Airport in New York City. More than 60,000 seizures of counterfeit and illegal goods were made last year at the facility.
“I am not surprised, unfortunately, any of these new type of drugs that we’re seeing, whether it be weight loss drugs or other drugs,” Sal Ingrassia, the port director overseeing U.S. Customs and Border Protection (CBP) at JFK, told CNBC. “We’ll see them either diverted, counterfeited or illegally shipped through this facility.”
According to CBP, since Jan. 1 the agency has made more than 198 seizures of medication labeled as Ozempic. Nine shipments of medication labeled as Wegovy were also seized, as well as one shipment labeled as Mounjaro.
The CBP seizures data doesn’t specify how much of that medication was real and diverted to the U.S. or counterfeit.
CNBC showed Ingrassia the Ozempic that it purchased from Laver Beauty, the package lacking the required refrigeration, and he said it was clear the shipment had “broken the legal supply chain.”
“This to me, is something that if we see, we are going to intercept and take action on. This is a dangerous product,” he said.
Ingrassia said he expects the number of interceptions of weight loss products to double this year over last.
And what happens to the seized items? Unless they’re part of an active investigation by the FDA, Ingrassia said, U.S. Customs isn’t allowed to destroy them, because the injection pens are categorized as medical devices. They are then sent back to the foreign supplier.
Illegal websites crackdown
Ingrassia said that for the most part, diverted products are ordered online or via social media.
“These are mostly individuals that are ordering this, going online and looking for a deal. And obviously taking a big risk by doing that. But we’ve also seen these products being ordered by doctors’ offices,” he said.
To go after the sellers of counterfeit or illegally diverted drugs, the pharmaceutical industry has teamed up with BrandShield, a cybersecurity company.
BrandShield CEO Yoav Keren showed CNBC various sites that the company flagged and that ultimately got shut down, including a Facebook account and a TikTok account that impersonated GLP-1 makers and sold versions of the drug.
Spokespeople for Meta, the parent company of Facebook and Instagram, and TikTok said their platforms do not allow the sale of prescription drugs and that the companies take action to remove those listings.
A Meta spokesperson in an email to CNBC said, “This is a challenge that spans platforms, industries, and communities which is why we work with law enforcement, regulators, and private industry to combat this problem. We continue to invest resources and further improve our enforcement on this kind of content.”
Keren said 250 sites identified by BrandShield as related to bogus weight loss products were removed last year, eight times the number in 2022.
“It’s kind of a whack-a-mole, but we’re on them. We’re chasing them, this is our technology, we find them very quickly,” he said.
The Turkey connection
Counterfeit Ozempic has been reported in 15 countries, according to the World Health Organization, which issued a global alert in June warning of the health risks of purchasing fake products.
For the U.S. government, it’s a big problem.
“We are seeing a lot of diverted medicines coming in from Europe and South America,” said Nicole Johnson, national program manager for the Intellectual Property Rights Coordination Center, which fights counterfeiting. “But for counterfeits, a lot of what we’re seeing currently in the United States is just the reuse of old Ozempic pens — so people can actually just take the original packaging and fill it with saline.”
Johnson said the top countries where counterfeits and diverted drugs originate are India, China, the United Kingdom, Mexico and Turkey. In Turkey, she says, government-subsidized pharmaceuticals have fueled the counterfeit drug market.
Istanbul may be known for the beauty of the Bosphorus, surrounded by stunning palaces and mosques. But it’s also one of the epicenters of the lucrative counterfeit drug trade, according to U.S. authorities who track counterfeit drugs.
“What the criminals normally do is they find something to exploit to make more money. So the pharmaceuticals were then bought up, and then sold throughout the world — something that was supposed to help people, and it’s being exploited,” Johnson said.
Last fall, the Turkish National Police conducted raids throughout Istanbul as part of a coordinated international crackdown.
Maziar Mike Doustdar, executive vice president of international operations for Novo Nordisk, agreed that Turkey has become a hot spot for pharmaceutical crime.
Counterfeiters have acquired sophisticated packaging equipment that is “on par with the original company equipment,” Doustdar said.
“They source the equipment from pretty much the same place as we or our competitors are sourcing it. So, they make the packaging look very, very, similar to the original product,” he said.
Direnc Bada, an Istanbul-based attorney who represents major pharmaceutical companies in Turkey, pointed to “an increasing amount of online channels promoting these products … and it’s forbidden in Turkey actually to sell these through online channels.”
FDA alert, complaints
In the U.S., the FDA announced in an alert in December that it had seized “thousands of units of counterfeit” Ozempic in the “legitimate U.S. supply chain.”
Asked about the status of the investigation into the counterfeit Ozempic, an FDA spokesperson said there were no updates to the original alert.
The risks in purchasing counterfeit drugs can be high. Given the delicate nature of the formulation and the specific shipping requirements for the drugs, consuming illegal versions can be dangerous to a person’s health.
“It’s one thing to counterfeit a luxury bag. It’s a very, very different thing when you counterfeit a medicine,” Doustdar said.
Reports of issues with weight loss drugs containing semaglutide, the active ingredient in Ozempic, or tirzepatide, the active ingredient in Mounjaro, have seen a sharp rise since 2019.
“This is a very serious problem for us as a pharma company, as an industry, because patient safety is our license to operate. And you’re playing with people’s safety,” Doustdar said.
“There is no good counterfeit,” he said.
— CNBC’s Eunice Yoon and Paige Tortorelli contributed to this report.
Credit: CNBC
Ever hear of tonsil stones?
Team Metabolic Health
They’re a common cause of bad breath and sore throats — and apparently a well-kept secret.
Recently, a friend asked me about tonsil stones. He has sore throats several times a year, which are instantly relieved by gargling to remove them. When I told him I thought tonsil stones were pretty rare, he asked: “Are you sure about that? My ear, nose, and throat doctor says they’re common as rocks.” (Get it? stones? rocks?)
It turns out, my friend and his doctor are on to something. Tonsil stones are surprisingly common and often quite annoying. Here’s what to know and do.

What are tonsil stones?
Tonsil stones (medical term: tonsilloliths) are small white or yellow deposits on the tonsils. They develop when bacteria, saliva, food particles, and debris from cells lining the mouth get trapped in tiny indentations called crypts.
They vary considerably between people, including:
Size. They may be so small that you can’t see them with the naked eye. Or they may grow to the size of gravel or, rarely, much larger.
Consistency. They’re often soft but may calcify, becoming hard as a rock. Hence, the name.
How long they last. Tonsil stones can last days to weeks, or may persist far longer before they break up and fall out.
How often they occur. New tonsilloliths may appear several times each month or just once or twice a year.
While they’re more likely to form if you have poor oral hygiene, good oral hygiene doesn’t provide complete protection. Even those who brush, floss, and see their dentists regularly can develop tonsil stones.
How common are tonsil stones?
You’ve heard of kidney stones and gallstones, right? Clearly, those conditions are better known than tonsil stones. Yet tonsil stones are far more common: studies suggest that up to 40% of the population have them. Fortunately, unlike kidney stones and gallstones, tonsil stones are usually harmless.
What are the symptoms of tonsil stones?
Often people have no symptoms. In fact, if tonsil stones are small enough, you may not even know you have them. When tonsil stones do cause symptoms, the most common ones are:
- Bad breath
- Cough
- Discomfort with swallowing
- Throat infections.
Who gets tonsil stones?
Anyone who has tonsils can get them. However, some people are more likely than others to form tonsil stones, including those who have tonsils with lots of indentations and irregular surfaces rather than a smooth surface
- Smoke
- Drink lots of sugary beverages
- Have poor oral hygiene
- Have a family history of tonsil stones.
How are tonsil stones treated?
That depends on whether you have symptoms and how severe the symptoms are.
If you have no symptoms, tonsil stones may require no treatment.
If you do have symptoms, gargling with salt water or removing tonsil stones with a cotton swab or a water flosser usually helps. Avoid trying to remove them with sharp, firm objects like a toothpick or a pen, as that can damage your throat or tonsils.
If your tonsils are inflamed, swollen, or infected, your doctor may prescribe antibiotics or anti-inflammatory medications.
Is surgery ever necessary?
Occasionally, surgery may be warranted. It’s generally reserved for people with severe symptoms or frequent infections who don’t improve with the measures mentioned above.
Surgical options are:
- Tonsillectomy, which is removing the tonsils
- Cryptolysis, which uses laser, electrical current, or radio waves to smooth the deep indentations in tonsils that allow stones to form.
Can tonsil stones be prevented?
Yes, there are ways to reduce the risk that tonsil stones will recur. Experts recommend the following:
- Brush your teeth and tongue regularly (at least twice a day: in the morning and before sleep).
- Floss regularly.
- Gargle with salt water after eating.
- Eliminate foods and drinks that contain a lot of sugar, which feeds bacteria that can help stones form.
- Don’t smoke, because smoking irritates and inflames tonsils, which can encourage stone formation. The same may apply to vaping, though there is limited research to rely upon.
The bottom line
Considering how common tonsil stones are and how bothersome they can be, it seems strange that they aren’t more well known. Maybe that’s because they often get better on their own, or people figure out how to deal with them without needing medical attention.
I hope you aren’t one of the many millions of people bothered by tonsil stones. But if you are, it’s good to know that they’re generally harmless and can be readily treated and prevented.
Now that you know more about them, feel free to spread the word: tonsil stones should be a secret no more.
Credit: health.harvard.edu/blog
How Broad Beans Can Help With Mental Health
Team Metabolic Health
It is often the tiniest of interventions that may deliver some respite. One of the most undervalued vegetables happens to be broad beans, which scientists have highlighted for their potential mental health benefits. This article examines these findings, glancing at how a broad bean may be an ally in supporting mental wellness.
What are broad beans?
Broad beans are nutritious green legumes that belong to the pea family. Generally known as the fava beans, these earthy-flavored legumes have been cultivated for thousands of years for their higher protein content, and the believed broad spectrum of potential health benefits they may bring to the table.

Image by JIANG HONGYAN via Shutterstock
Broad beans’ nutritional benefits
Among their vast nutritional content, broad beans are packed with plant protein. In fact, one cup of cooked fava beans provides approximately 12.9 grams of protein, which is essential for the repair and growth of our muscles.
Around 9.18 grams of fiber can be found in a single cup of cooked broad beans. Nutritional health science has shown ample evidence of the role of fiber in digestion, the support of our gut health, and the potential contribution to blood glucose level regulation.
Broad beans’ nutritional value is emphasized by their abundance in folate, which has an array of functions such as DNA synthesis, infant development during pregnancy, and support for brain health. These beans also contain vitamin C, a nutrient treasured by many of us today for its potential immune system support.
Further highlighting their benefits, fava beans are high in iron, magnesium, and potassium. These minerals are research-proven to play an essential role in preventing anemia, supporting muscle and nerve functioning, and regulating blood pressure, respectively.
Broad beans’ nutrition gains are quite vast, as they’ve also been established to contain some useful antioxidant compounds, which include flavonoids and phenolic acids that are important in supporting the management of oxidative stress and are recognized as compounds that may have anti-inflammatory properties.
The science behind broad beans and mental health
Leading the charge in integrating broad beans into everyday nutrition is Nadia Mohd-Radzman, a Cambridge research scientist. Her research highlights the resilience of broad beans in agriculture and their potential contribution to the health of their rich nutrient profile.
In advocating for the nutritional benefits of broad beans, Mohd-Radzman seeks to highlight their potential as a complementary part of a healthy and balanced diet that may support both our physical and mental well-being.
We have a major problem with growing numbers of young people experiencing mental health problems in the UK today, and helping them eat a proper, healthy diet is going to be crucial in tackling this. The broad bean will be our first line of attack.
Stress often creeps into our lives, potentially affecting our cognitive function and emotional health. The nutrients in broad beans hence show promise to potentially contribute to the reduction of stress. The nutritional properties of these beans may work to support stress, cognitive performance, and supporting our overall mental health.
Associations between some of the micronutrients found in board beans and mental health exist in some of the scientific literature. Broad beans are relatively high in magnesium, with some literature reviews suggesting that magnesium may help relieve perceived stress levels in adults with moderate to severe stress levels and hypomagnesemia. Moreover, it is noted that nearly 30% of severely depressed inpatients have folate deficiency, and some studies suggest that folate may play a role in cognitive health maintenance.
However, the scientific evidence on these certain micronutrients is too limited to validate their efficacy in mental health support. Also, most of the current research is focused on the specific micronutrient supplementation in certain groups rather than the intake of micronutrients from broad beans; thus the potential mental health effects of increased natural sources of the micronutrients are less scientifically assessed.
It is crucial to recognize that while these micronutrients show some promise in supporting mental well-being, they may be just one piece of a much larger picture. Depression, anxiety, and other mental health challenges are far more complex, usually requiring a multifaceted strategy that involves medical treatment, therapy, and support from our loved ones. Broad beans can only be a small addition to a healthy and balanced diet with nutritional properties to support overall mental health, but they are not a way to manage or treat any mental health disorders.
Important
If you experience mental health challenges, it is important to consult with a medical professional who can assess your mental health and provide personalized advice on the best methods for managing your specific situation.
Broader implications for mental health
Let’s dig a bit deeper into the suggested potential benefits of broad beans and how they may extend beyond well-known micronutrients.
Broad beans represent a rich source of levodopa, otherwise known as L-Dopa, an amino acid that acts as a precursor to dopamine. Some scientific literature associates low dopamine levels and dysregulation of dopamine with depressive disorders. Therefore, as a precursor to dopamine, L-Dopa may play a role in supporting mental health.
Some studies suggest that L-Dopa may play a role in reward circuitry in people with depressive disorders and anhedonia (reduced ability to experience pleasure). However, another study discussed that although L-Dopa levels may increase from broad bean intake, consuming extremely large quantities of fava beans may cause digestive side effects like flatulence.
Due to the current lack of comprehensive scientific evidence, the significance of broad beans for mental health or neurodegenerative disease management requires further exploration. Therefore, the effectiveness of broad beans in supporting mental health cannot be fully verified at this time.
Practical ways to incorporate broad beans into your diet
Think about starting your day with a vibrant broad bean salad, its fresh mint and tangy lemon dressing waking up your senses. Or picture a creamy broad bean hummus, perfect for a mid-day snack that nourishes your body and mind. For dinner, a quick broad bean stir-fry can bring comfort and joy after a long day with its flavors dancing on your tongue.
You don’t need to be a master chef to enjoy broad beans in your diet. Many recipes online can guide you step-by-step in preparing broad beans in delicious ways, whether in soups, stews, or simply sprinkled over toast. The possibilities are endless!
Dietary recommendations
Balance is key to everything in life. To fully gain the potential nutritional benefits of broad beans, it’s important to remember that when incorporating them into your diet.
Some of the dietary recommendations include:
Serving size. A typical serving is about 1/2 cup of cooked broad beans. The nutrient content can vary with the preparation method (e.g., cooked vs. raw), so adjust based on your needs and consult a healthcare professional for personalized advice.
Balanced diet. Embrace broad beans as a part of a balanced diet that contains a variety of fruits, vegetables, whole grains, and lean proteins.
Hydration. Staying hydrated is crucial, as water supports metabolism, digestion, and overall health.
Broad beans vs. other nutritional choices
When considering diet’s impact on mental health, specific foods can play a unique role. Legumes, including broad beans, offer a range of nutrients that may contribute to mental well-being. In particular, broad beans stand out among their leguminous counterparts for their potential cognitive and mental health benefits.
Broad beans vs. other legumes
Intake of raw vegetables, including legumes, is found to have a strong association with better mental health. Among legumes, broad beans stand out alongside lentils, chickpeas, and black beans. While each of these foods offers unique benefits and should be included in a healthy diet, broad beans may provide specific advantages for mental health when combined with a balanced diet and other healthy lifestyle practices.
While lentils and chickpeas excel in protein and fiber and contain decent amounts of magnesium and folate, they lack the L-Dopa found in broad beans that may contribute to cognitive function and mental health.
Broad beans vs. supplements
Nutritional supplements can be beneficial, particularly in cases of nutrient deficiency. But while supplements can help fill nutritional gaps and may be recommended by a healthcare provider in certain situations, it is generally advised to prioritize a balanced diet with a variety of nutrient-rich foods to support overall health, including mental health.
In the case of whole foods like broad beans, there is a symphony of nutrients backing their consumption. Their fiber, protein, folate, magnesium, and antioxidants are all acting collectively to potentially support mental health.
Holistic approach to mental health management
Acupuncture, mindfulness, and dietary changes can be extremely impactful in the management of mental health. Adding broad beans to the punch alongside a balanced diet may fit well into a CAM strategy and provide a natural and holistic approach to dealing with mental health issues.
Potential side effects and precautions
Moderation is important, as even beneficial foods can have negative effects if consumed in excess or without considering their impact. Broad beans are no exception. While they offer several potential benefits, it’s important to be aware of possible side effects and take necessary precautions.
Allergies and sensitivities
On rare occasions, broad beans can elicit allergic reactions and cause symptoms like itching, swelling, hives, and even anaphylaxis. Always read labels to avoid unexpected surprises. It’s advisable to consult with your healthcare provider before incorporating any new foods into your diet.
Additionally, fava beans can trigger a genetic condition called favism, named after the very beans themselves. This genetic condition stems from a deficiency in an enzyme known as glucose-6-phosphate dehydrogenase (G6PD), which turns these beans into possible health hazards for some people by inducing hemolytic anemia.
G6PD deficiency precaution
If your family history hints at G6PD deficiency, or if you’ve been diagnosed with the disease, broad beans should be avoided, as they can have serious negative implications on your health.
Interaction with medications
The high mineral content in broad beans can be a blessing or a challenge. For those on blood pressure medications, this means monitoring your potassium levels carefully. Additionally, although they may help support dopamine levels, broad beans may interact with Parkinson’s medications. If you’re on any such medications, it’s best to consult with your healthcare provider before making any dietary changes.
Bottom line
Nutrition and mental health are closely connected. While there is some promising evidence regarding the potential role of micronutrients and L-Dopa found in broad beans for mental health, the research is still too limited to confirm their impact. However, due to their nutritional content, broad beans can be a beneficial addition to a healthy and balanced diet.
FAQ
- Can broad beans be eaten raw?
- Broad beans should not be eaten raw. The raw pods contain certain compounds that hinder nutrient absorption and are relatively tough to digest. Proper cooking helps in neutralizing these compounds, making them more palatable and easier for digestion.
- Can eating broad beans improve sleep quality?
- Although broad beans have no direct association with better sleep, the high content of magnesium may support the nervous system. This alongside other sleep hygiene practices may help with a good night’s sleep.
Key takeaways:
- Broad beans are green legumes rich in useful nutrients such as folate, magnesium, protein, and fiber, among others. These nutrients provide well-rounded support for overall physical health and may contribute to mental well-being.
- The L-Dopa in broad beans may increase dopamine levels, providing a natural way of supporting your mood.
- Enjoying the benefits of broad beans while being mindful of potential allergic reactions and medication interactions is the best approach. Consult with your healthcare provider for safe and balanced consumption.
Credit: healthnews.com
Ozempic’s cousin drug liraglutide is about to get cheaper. But how does it stack up?
Team Metabolic Health
Fourteen years ago, the older drug cousin of semaglutide (Ozempic and Wegovy) came onto the market. The drug, liraglutide, is sold under the brand names Victoza and Saxenda.
Patents for Victoza and Saxenda have now expried. So other drug companies are working to develop “generic” versions. These are likely be a fraction of current cost, which is around A$400 a month.
So how does liraglutide compare with semaglutide?
How do these drugs work?
Liraglutide was not originally developed as a weight-loss treatment. Like semaglutide (Ozempic), it originally treated type 2 diabetes.
The class of drugs liraglutide and semaglutide belong to are known as GLP-1 mimetics, meaning they mimic the natural hormone GLP-1. This hormone is released from your small intestines in response to food and acts in several ways to improve the way your body handles glucose (sugar).
How do they stop hunger?
Liraglutide acts in several regions of the unconscious part of your brain, specifically the hypothalamus, which controls metabolism, and parts of the brain stem responsible for communicating your body’s nutrient status to the hypothalamus.
Its actions here appear to reduce hunger in two different ways. First, it helps you to feel full earlier, making smaller meals more satisfying. Second, it alters your “motivational salience” towards food, meaning it reduces the amount of food you seek out.
Liraglutide’s original formulation, designed to treat type 2 diabetes, was marketed as Victoza. Its ability to cause weight loss was evident soon after it entered the market.
Shortly after, a stronger formulation, called Saxenda, was released, which was intended for weight loss in people with obesity.
How much weight can you lose with liraglutide?
People respond differently and will lose different amounts of weight. But here, we’ll note the average weight loss users can expect. Some will lose more (sometimes much more), others will lose less, and a small proportion won’t respond.
The first GLP-1 mimicking drug was exenatide (Bayetta). It’s still available for treating type 2 diabetes, but there are currently no generics. Exenatide does provide some weight loss, but this is quite modest, typically around 3-5% of body weight.
For liraglutide, those using the drug to treat obesity will use the stronger one (Saxenda), which typically gives about 10% weight loss.
Semaglutide, with the stronger formulation called Wegovy, typically results in 15% weight loss.
The newest GLP-1 mimicking drug on the market, tirzepatide (Mounjaro for type 2 diabetes and Zepbound for weight loss), results in weight loss of around 25% of body weight.

People often regain weight when they stop taking the drug. Mohammed_Al_Ali/Shutterstock
What happens when you stop taking them?
Despite the effectiveness of these medications in helping with weight loss, they do not appear to change people’s weight set-point.
So in many cases, when people stop taking them, they experience a rebound toward their original weight.
What is the dose and how often do you need to take it?
Liraglutide (Victoza) for type 2 diabetes is exactly the same drug as Saxenda for weight loss, but Saxenda is a higher dose.
Although the target for each formulation is the same (the GLP-1 receptor), for glucose control in type 2 diabetes, liraglutide has to (mainly) reach the pancreas.
But to achieve weight loss, it has to reach parts of the brain. This means crossing the blood-brain barrier – and not all of it makes it, meaning more has to be taken.
All the current formulations of GLP-1 mimicking drug are injectables. This won’t change when liraglutide generics hit the market.
However, they differ in how frequently they need to be injected. Liraglutide is a once-daily injection, whereas semaglutide and tirzepatide are once-weekly. (That makes semaglutide and tirzepatide much more attractive, but we won’t see semaglutide as a generic until 2033.)
What are the side effects?
Because all these medicines have the same target in the body, they mostly have the same side effects.
The most common are a range of gastrointestinal upsets including nausea, vomiting, bloating, constipation and diarrhoea. These occur, in part, because these medications slow the movement of food out of the stomach, but are generally managed by increasing the dose slowly.
Recent clinical data suggests the slowing in emptying of the stomach can be problematic for some people, and may increase the risk of of food entering the lungs during operations, so it is important to let your doctor know if you are taking any of these drugs.
Because these are injectables, they can also lead to injection-site reactions.

Gastrointestinal side effects are most common. Halfpoint/Shutterstock
During clinical trials, there were some reports of thyroid disease and pancreatitis (inflammation of the pancreas). However, it is not clear that these can be attributed to GLP-1 mimicking drugs.
In animals, GLP-1 mimicking drugs drugs have been found to negatively alter the growth of the embryo. There is currently no controlled clinical trial data on their use during pregnancy, but based on animal data, these medicines should not be used during pregnancy.
Who can use them?
The GLP-1 mimicking drugs for weight loss (Wegovy, Saxenda, Zepbound/Mounjaro) are approved for use by people with obesity and are meant to only be used in conjunction with diet and exercise.
These drugs must be prescribed by a doctor and for obesity are not covered by the Pharmaceutical Benefits Scheme, which is one of the reasons why they are expensive. But in time, generic versions of liraglutide are likely to be more affordable.
Credit: The Conversation
Understanding Krishnasportsnews: Dosage and Route of Administration for Sportsmen
Understanding Krishnasportsnews: Dosage and Route of Administration for Sportsmen
In the world of sports, performance enhancement and recovery are crucial aspects that athletes focus on. One emerging topic gaining attention is the krishnasportsnews dosage and route of administration for sportsmen. This article explores the significance of proper dosage and administration routes for athletes aiming to optimize their performance safely and effectively.
The Importance of Dosage in Sports
Dosage plays a critical role in how well an athlete responds to any substance or supplement. An incorrect dosage can lead to adverse effects rather than the desired benefits. It is essential for sportsmen to understand the recommended krishnasportsnews dosage tailored to their specific needs.
Factors Influencing Dosage
Several factors influence the appropriate dosage for sportsmen, including:
- Body weight and composition
- Type of sport and intensity of training
- Individual health conditions
- Response to previous supplementation
Route of Administration: Finding the Best Method
The route of administration refers to how a substance is delivered into the body. Different methods can affect the absorption rate and overall efficacy of supplements. For sportsmen, commonly used routes include:
- Oral Administration: Pills, capsules, or liquid forms taken by mouth are popular due to convenience and ease of use.
- Intravenous (IV) Administration: Directly delivering nutrients into the bloodstream can ensure immediate effects, but it requires medical supervision.
- Topical Application: Creams or gels applied to the skin offer localized effects, which might be beneficial for recovery from injuries.
Choosing the Right Route
When considering the krishnasportsnews route of administration, athletes should evaluate which method aligns best with their training regimen, lifestyle, and health status. Consulting with healthcare professionals can provide personalized recommendations.
Safety and Regulations
Safety is paramount when it comes to performance-enhancing substances. Athletes must ensure they comply with regulations set forth by sports governing bodies to avoid disqualification or bans. Understanding the legal implications of using certain dosages or administration routes is essential for maintaining integrity in https://krishnasportsnews.com/product/alphabolin-vial/ sports.
Consultation and Monitoring
Regular consultation with sports nutritionists or healthcare providers is advisable for athletes. Monitoring the effects of dosages and adjusting the krishnasportsnews dosage and route of administration based on performance and health feedback can lead to optimal outcomes.
Conclusion
In conclusion, the krishnasportsnews dosage and route of administration for sportsmen is a vital aspect of enhancing athletic performance responsibly. By understanding the importance of correct dosages and choosing the right administration routes, athletes can maximize their training efforts while prioritizing their health and adherence to sports regulations.
Are Stroke Survivors Getting Too Many Sedatives Like Xanax, Valium?
Team Metabolic Health
Doctors might be overprescribing sedatives to stroke survivors, a new study warns.
About 5% of people are prescribed a benzodiazepine following a stroke, to help calm anxiety and improve sleep, researchers found. Benzodiazepine meds include Valium, Ativan and Xanax.
But these prescriptions often are for pills that last longer than a week, which could hamper a person’s recovery and increase their risk of addiction.
“We found a pattern of potential oversupply with these initial benzodiazepine prescriptions, which would be enough for patients to become long-term users or possibly addicted,” said researcher Julianne Brooks, a data analytics manager at Massachusetts General Brigham in Boston. “The benzodiazepine prescriptions given under these circumstances may lead to dependence.”

Credit: Adobe
For the study, researchers analyzed a decade’s worth of Medicare claims data on first-time prescriptions for benzodiazepines among more than 120,000 stroke victims aged 65 and older.
“For this older age group, guidelines recommend that benzodiazepine prescriptions should be avoided if possible,” Brooks said.
These sedatives increase the risk of falls, broken bones, memory problems, confusion and other harmful effects, the researchers said.
“However, there may be cases where benzodiazepines are prescribed to be used as needed,” Brooks noted. “For example, to treat breakthrough anxiety, a provider may prescribe a few pills and counsel the patient that the medication should only be used as needed.”
Researchers found that about 5% of patients were started on a benzodiazepine within 90 days of their stroke.
Lorazepam (Ativan) and alprazolam (Xanax) were most frequently prescribed, to 40% and 33% of patients, respectively.
Three-quarters of these prescriptions were for a supply of over seven days, and more than half for a supply between 15 and 30 days, researchers found.
That’s too many pills, researchers contend.
“Benzodiazepines may inhibit recovery and rehabilitation,” Brooks said.
“Although the overall prescription rate decreased slightly over 10 years, this prescription pattern is still a problem,” Brooks added. “It’s concerning because older adults are vulnerable to overprescribing and adverse outcomes.”
Prescription rates were higher among women (5.5%) than men (3.8%).
Overall, prescription rates were highest in the Southeast (5.1%) and lowest in the Midwest (4%).
“The Southeast region is the stroke belt with a higher rate of strokes, so that could explain some differences in care in that region,” Brooks said.
The findings were published Oct. 17 in the journal Stroke.
The American Geriatrics Society recommends avoiding benzodiazepines in all older adults due to the risk of cognitive impairment, delirium, falls, fractures and motor vehicle crashes, the researchers noted.
“Other guidelines also suggest behavioral interventions such as cognitive behavior therapy for insomnia, antidepressant medications for anxiety disorders and trying non-pharmaceutical interventions first,” Brooks said in a journal news release.
However, the researchers said more studies are needed to figure out if there is a safe level for prescribing benzodiazepines to seniors.
Credit: healthday.com
Is your heart attack risk going up because of factors other than cholesterol? Watch your triglycerides
Team Metabolic Health
High triglyceride levels often come from consuming excessive fats — from oils, dairy and animal products
Whenever we talk about heart attacks caused by plaque deposits in the blood vessels, we always talk about controlling cholesterol. Truth is while cholesterol gets most of the attention, triglycerides are another significant risk factor. In fact, when their levels rise up above 100 mg/dL, they too begin accelerating plaque buildup in the arteries.
Elevated triglyceride levels can be harmful to heart health and significantly increase the risk of cardiovascular diseases. (Photo credits: Pexels)
What are triglycerides?
Triglycerides are a type of fat found in the blood. They play a crucial role in storing and transporting energy throughout the body. However, elevated triglyceride levels can be harmful to heart health and significantly increase the risk of cardiovascular diseases.
How do Triglycerides form plaques?
One of the primary ways elevated triglycerides impact the heart is by thickening and hardening artery walls, a condition known as atherosclerosis. This process leads to the buildup of fatty deposits or plaques, which narrow the arteries, restrict blood flow, and increase the risk of heart attacks and strokes. High triglyceride levels are often accompanied by low levels of HDL (good cholesterol) and high levels of LDL (bad cholesterol), creating a perfect storm for cardiovascular complications.
Moreover, high triglycerides are closely linked to other health conditions, such as obesity, metabolic syndrome, type 2 diabetes, and hypertension, all of which further exacerbate the risk of heart disease. Elevated triglycerides can also contribute to pancreatitis, a painful inflammation of the pancreas, adding another layer of health complications.
Once you eat, your metabolism breaks down your food so that your body can draw energy. When we consume excess calories—especially from sugary foods, refined carbohydrates and unhealthy fats—the body converts these into triglycerides, which are stored in fat cells for future use. While this storage mechanism is essential for energy balance, consistently high levels lead to serious health issues.
The breakdown of triglycerides leaves some byproducts or “remnant particles.” These include leftover bits of cholesterol and fatty acids, which had been bunched together with triglycerides. These float around, trigger inflammation of your arteries that leads to plaque buildup. So, even though triglycerides don’t stick to your artery walls, they are the reason that arteries narrow and breakaway particles block them in the first place.
Why do triglycerides rise?
High triglyceride levels often come from consuming excessive fats—particularly from sources like oils, dairy, and animal products. However, even seemingly healthy foods like nuts can be problematic for heart patients. Almonds, walnuts, and cashews, while nutritious, are high in fats nevertheless and should be had in moderation or avoided by those with heart disease. It’s essential to focus on a diet low in fats and oils to reduce the risk of blockages.
Managing triglyceride levels is crucial because it can prevent these conditions from progressing. Regular physical activity, a balanced diet rich in omega-3 fatty acids, and avoiding excessive sugars and trans fats are effective ways to maintain healthy triglyceride levels. For some, medications may also be necessary to bring levels into a safer range. In essence, controlling triglycerides is essential for maintaining not just heart health but overall wellness and longevity.
Credit: The Indian Express
Anadrol Oxymetholon Wirkung, Dosierung, Nebenwirkungen Und Alternativen
Anadrol Oxymetholon Wirkung, Dosierung, Nebenwirkungen Und Alternativen
Alle anabolen Steroide senken den natürlichen Testosteronspiegel, die negativen Auswirkungen von Anadrol auf den Testosteronspiegel sind jedoch dramatisch. Das ist ein anderes Erscheinungsbild als bei heutigen Bodybuildern, die mehr androgene Verbindungen einnehmen und schnell eine Glatze bekommen. CrazyBulk’s Anadrole könnte als eine sicherere und legale Alternative zu dem anabolen Steroid Anadrol dienen. Anadrole zielt darauf ab, die muskelaufbauenden Effekte von Anadrol (Oxymetholon) zu duplizieren, ohne die schweren Nebenwirkungen, die Ihre langfristige Gesundheit schädigen könnten. Aufgrund seines Missbrauchs und der Besorgnis über die Lipidtoxizität wurde Oxymetholon jedoch aus dem klinischen Gebrauch genommen.
Zusätzliche Beschreibung Danabol
Wer nicht auf anabole Steroide verzichten und diese kaufen möchte, um bessere Ergebnisse zu erzielen, sollte sich für eine legale Alternative entscheiden. Es gibt genügend Produkte, die teilweise sogar mehr Effektivität hervorbringen und die es zudem kostengünstiger gibt. Der Preis von rund forty five Euro ist im Preis- Leistungs-Verhältnis kaum zu unterbieten, im Gegensatz zu anderen teureren Erzeugnissen. Sie als Kunde, bekommen nicht nur hochwertige Produkte, sondern Anadrole verfügt über keine Nebenwirkungen und ist die legale Antwort zu Anadrol. Fast der gesamte Anteil der Wirkstoffanteile durchläuft das Organ, ohne allerdings dabei zerstört zu werden. Anadrol wird zum Masseaufbau genutzt und ist ein Wirkstoff, welcher in hohen Dosierungen zu Östrogen konvertieren kann.
Nach kurzer Zeit wird sich herausstellen, welche Dosierung am besten passt und, ob diese über 50 mg liegen darf. Nicht zu vergessen ist, dass trotz einer Einnahme von Oxymetholon oder eben Anadrol, eine ausgewogene und abwechslungsreiche Ernährung, unbedingt dazu gehört. Gerade beim Bodybuilding wird Anadrol wegen seiner ausgeprägten anabolen Wirkung, gern eingesetzt. Der Grund hierfür Fettverbrennung tabletten (Fettverbrenner) online bestellen liegt in dem Kriterium, dass es sehr stark Wasser zurückhält und die Muskeln sich dadurch bedingt, optisch verändern. Nach der Erfindung von sicheren Analoga (synthetisches Erythropoetin), kam Oxymetholon erst gar nicht zur medizinischen Verwendung.
Brutal Anadrol Von Biotech Usa
Folglich können Professionelle Bodybuilder in Deutschland von uns ihren kompletten Bedarf für die Wettkampfvorbereitung und die Aufbaukur aus einer Hand beziehen. Für Anfänger haben wir fertige Steroidkuren als Bundle mit dazugehörigen PCT Medikamenten im Angebot. Ausnahmslos Originale anabole Steroide und Wachstumshormone sowie Antiöstrogene. Vielmehr sehen wir uns aber als breit aufgestellten und soliden Lieferanten für hochwertige Markensteroide. Zudem werden alle Steroids und weiteren Produkte aus unserem Shop diskret aus Deutschland versendet. Anadrol erzeugt tatsächlich androgene Nebenwirkungen, obwohl es auf dem Papier eine niedrige androgene Einstufung hat (45).
Anadrol 50 – The Cause Why You Should Run An Anadrol Cycle
- Diese Nebenwirkungen wurden auch wieder rückgängig gemacht, nachdem sie die Einnahme von Anadrol beendet hatten.
- Diese Anwendung ermöglicht gute Erfolge und sollte mit einer guten Ernährung ergänzt werden, um den Körper beim Muskelaufbau zu unterstützen.
- Anadrol ist ein von DHT abgeleitetes Steroid, aber es wandelt sich auch in Dihydrotestosteron um, das Hormon, das für Haarausfall auf der Kopfhaut verantwortlich ist.
- Obwohl Danabol viele mögliche Nebenwirkungen hat, sind sie mit einer Dosierung von bis zu 20 mg / Tag selten.
So kannst Du auch deine gewonnene Muskelmasse langfristig behalten und deine Testoproduktion wieder ankurbeln. Aber auch während des Steroid-Zyklus solltest du deinen Körper – insbesondere die Leber – effektiv mit einer On-Cycle-Therapy unterstützen. Die Menge an Anapolon , die ein Sportler für eine gute und sichere Wirkung konsumieren muss, sollte in jedem Fall individuell bestimmt werden. Hier kommt es auf das Gewicht, den Trainingszustand des Athleten und dessen Zielvorstellungen an. Anfänger können sich auf eine Dosis von etwa zehn bis 15mg des oralen Steroids einstellen, erfahrenere Sportler können auch bis zu 50mg oder mehr am Tag aufnehmen. Eine Kur mit Androl erfolgt in der Regel über etwa vier bis sechs Wochen und sollte zum Schutz des Körpers danach beendet werden.
Can Constipation Cause Back Pain?
Team Metabolic Health
Back pain is common and is usually caused by an injury or age-related degenerative conditions affecting the spine, spinal nerves, or muscles in the back. But injuries and age aren’t the only causes of back pain. Have you ever had back pain that seems unrelated to any injury? Surprisingly, this unexpected back pain may be a side effect of constipation.
Find out more about constipation-related back pain and what you can do about it.
What is constipation?
Almost everyone experiences constipation at some point in their life. The general medical definition for constipation is when you have three or fewer bowel movements a week, passing stool that’s dry and hard. But if your usual bowel movement schedule isn’t like others and is usually less frequent, true constipation is when there’s a change in your normal bowel movements.
Some people poop several times a day, while others poop only a few times a week. According to the American Society of Colon & Rectal Surgeons (ASCRS), individual constipation is pooping less often than normal or passing stool that’s rock hard and requires excessive straining. A slowdown in the movement of food waste through the digestive tract, or more specifically the colon, causes constipation.
Your digestive system absorbs as much nutrition as possible — carbs, protein, fat, vitamins, minerals, and other health-promoting nutrients — from the food you eat as it moves its way through. The food waste that reaches the colon is made up of nondigestible fibers and water.
A lot happens in the colon as the food waste moves through. The microorganisms that live in this part of your digestive tract feed off the fiber and make essential nutrients, the waste collects toxic substances for removal, and any remaining water is reabsorbed. The longer it takes for stools to move through the colon, the more water it removes, creating the dry, hard, and difficult-to-pass stool.
Constipation has many causes, including a change in diet, alterations in your usual routine, stress, or certain medications. For most people, constipation clears up on its own within a few days. However, if you continue to have infrequent or hard-to-pass poop for several weeks, you may have chronic constipation.
Symptoms of constipation
- Common constipation symptoms mostly center around your bowel movements and include:
- Having fewer than three bowel movements a week or changes to your normal bowel habits
- Passing rock-like pieces of stool (hard and small)
- Straining to pass stool
- Experiencing pain during bowel movements
- Lingering urge to poop after having a bowel movement
- More serious symptoms of constipation include:
- Inability to pass gas
- Bleeding during a bowel movement
- Blood in stool
- Constant stomach pain
- Not passing stool
- Vomiting
- Fever
On top of these symptoms, constipation may cause back pain, seeming completely unrelated to your tummy issues.
Can constipation cause back pain?
In a nutshell, constipation can cause back pain, especially in the lower back. The pain may occur because of a buildup of stool in the large intestines, leading to swelling that puts pressure on the spinal cord or spinal nerves.
Preliminary research also shows an association between constipation, an imbalance in the gut microbiome, and back pain. People who experience constipation are more likely to have an imbalance in bacteria in the gut and more severe lower back pain than people without constipation, according to a 2018 study published in Anesthesiology and Pain Medicine. The researchers theorize that the imbalance in the microbiome may affect communication between the gut and brain, influencing and exacerbating pain sensations. But this is preliminary evidence and more research is needed to better understand the connection between constipation, chronic back pain, and the microbiome.
Lower back pain is also a symptom of fecal impaction, a severe form of constipation that requires immediate medical attention. It’s a type of bowel obstruction where dry, hard stool gets stuck in the rectum, the last section of the large intestine that holds stool before elimination. Abdominal pain, bloating, and difficulty passing stool are other symptoms you may have with fecal impaction. Without immediate treatment, the impacted stool may tear through the intestinal wall, leading to an infection.
Conditions that cause both constipation and back pain
Constipation and back pain are symptoms that occur from any number of causes. Experiencing both symptoms at the same time can help pinpoint the underlying cause.
Constipation is one of many symptoms that affect people with irritable bowel syndrome (IBS), a functional gastrointestinal disorder where the gut and brain don’t work together as they should. Symptoms vary in type and severity with irritable bowel syndrome but may include abdominal pain, bloating, and changes in bowel habits.
Other conditions that can cause both constipation and back pain include:
If you have chronic pain, taking certain medications to manage your discomfort may cause or worsen constipation.
When to see a healthcare provider
If you have severe abdominal pain, difficulty passing stool, or signs of dehydration related to your constipation, seek immediate medical attention. You should also make an appointment with your doctor if you have severe constipation and back pain that lasts longer than a few weeks.
Severe back pain, numbness and tingling in the legs, difficulty controlling bowel movements (incontinence), or unexplained weight loss are also symptoms of concern that should benefit from a doctor’s evaluation.
Self-care for constipation and back relief
Making changes to your lifestyle may help you manage both your constipation and back pain. Increasing your fiber intake and managing stress may help relieve both symptoms. More fiber adds bulk to stool, making it easier to pass, reducing buildup and pressure. Stress may trigger IBS and exacerbate back pain and constipation.
Drinking plenty of water to stay hydrated can help prevent constipation. You also want to limit foods with little to no fiber, such as snack foods, fast food, and processed food.
Getting regular exercise also benefits constipation and back pain. Walking and yoga are good forms of physical activity that can improve bowel function and reduce symptoms of constipation. Exercise also releases the body’s natural painkillers to help reduce chronic back pain.
Your doctor may also recommend a stool softener and a bathroom routine that helps you find relief from constipation. Natural stool softeners like prunes, flaxseed, and psyllium may also help.
Final word
Constipation and lower back pain are common health complaints. Though back pain has many causes, you may not connect your chronic pain with your infrequent bowel movements, but constipation can cause lower back pain. Improving bowel regularity may help you get relief from your back pain, but you should talk to your doctor if your constipation persists.
FAQ
- What does constipation back pain feel like?
- Constipation back pain may cause a dull ache in the lower back. Over time, this may worsen and spread to the abdomen.
- How do I know if my back pain is bowel-related?
- Having a dull ache in your lower back and experiencing constipation at the same time may suggest that the two may be connected. Your doctor can truly determine if your back pain is bowel-related. They diagnose the cause of your pain based on symptoms and testing.
- Where is constipation pain located?
- Constipation pain usually affects the lower abdomen. You may feel pressure or bloating, but symptoms can vary.
Key takeaways:
- Constipation is when you have fewer bowel movements than usual or you strain to pass hard and dry stool.
- Constipation can cause back pain from pressure on the spinal cord or nerves due to a buildup of stool in the lower part of the large intestine.
- Constipation and back pain are symptoms with many causes and you should talk to your doctor when either symptom persists.
- Eating more fiber, drinking more water, and regular exercise can benefit both constipation and back pain.
Credit: healthnews.com
Off-label semaglutide, tirzepatide lower HbA1c and body weight in type 1 diabetes
Team Metabolic Health
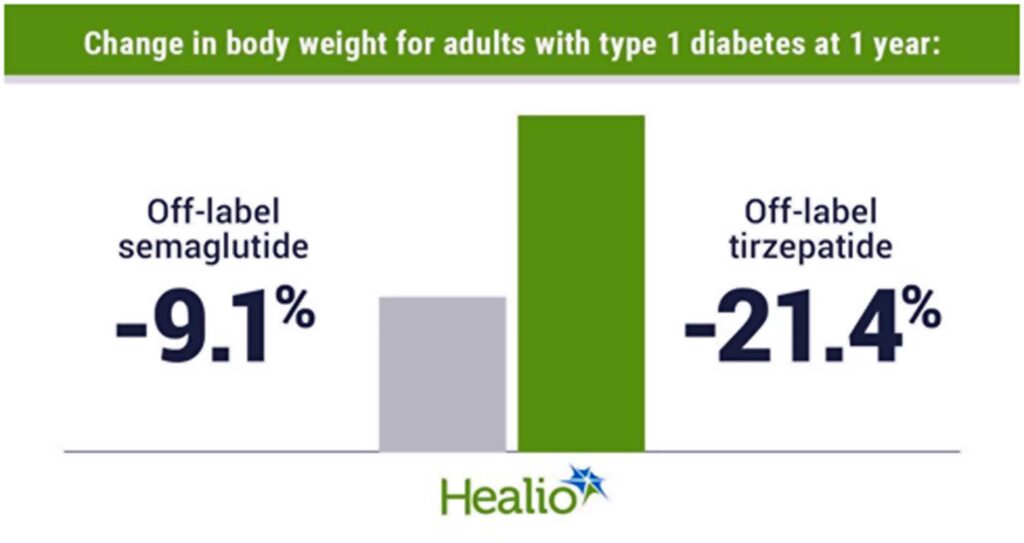
Adults with type 1 diabetes had significant declines in body weight at 1 year of off-label semaglutide and tirzepatide use.
Use of both medications was associated with reductions in total daily insulin dose.
Adults with type 1 diabetes using either semaglutide or tirzepatide off-label had greater decreases in body weight and HbA1c than those not treated with either medication, according to a speaker.
As Healio previously reported, researchers at the Barbara Davis Center for Diabetes at University of Colorado Anschutz Medical Campus found adults with type 1 diabetes and overweight or obesity using tirzepatide (Mounjaro/Zepbound, Eli Lilly) off-label had a 0.67 percentage point reduction in HbA1c and an 18.5% decrease in body weight at 1 year. At the European Association for the Study of Diabetes annual meeting, University of Colorado researchers presented more data from their institution of adults with type 1 diabetes who used tirzepatide as well as semaglutide (Ozempic/Wegovy, Novo Nordisk) off-label.
Data were derived from Snell-Bergeon J, et al. OP 43. Presented at: European Association for the Study of Diabetes Annual Meeting; Sept. 9-13, 2024; Madrid.
“Off-label semaglutide and tirzepatide treatment resulted in significant weight loss and improved glycemic control in adults with type 1 diabetes, with no reported hospitalization for hypoglycemia or diabetic ketoacidosis,” Janet Snell-Bergeon, PhD, professor of pediatrics at the Barbara Davis Center for Diabetes at the University of Colorado Anschutz Medical Campus, said during the presentation.
Researchers conducted a retrospective chart review of 50 adults with type 1 diabetes and overweight or obesity who used semaglutide off-label and 50 adults who used tirzepatide off-label. Propensity score matching was used to compare data from semaglutide and tirzepatide users with 50 controls with type 1 diabetes and overweight or obesity who were not treated with either medication. Changes in BMI, body weight and HbA1c were assessed over a 1-year period.
Reductions in weight, HbA1c
Adults using tirzepatide had a 7.5 kg/m2 decline in BMI and semaglutide users a 3 kg/m2 decrease in BMI from baseline to 12 months (P for treatment difference < .0001). The tirzepatide group had a significantly greater reduction in BMI than controls starting at 3 months and continuing until the end of the study, whereas semaglutide users had a significantly greater decrease in BMI than controls beginning at 6 months and continuing through 1 year.
The tirzepatide group lost 21.4% of their body weight from baseline to 1 year and the semaglutide group achieved a 9.1% weight reduction in that same period (P for treatment difference < .0001). A weight loss of 10% or more at 1 year was achieved by 87% of adults using tirzepatide and 47% of those using semaglutide compared with no participants in the control group (P < .001).
Adults using semaglutide had a 0.54 percentage point decline in HbA1c at 1 year compared with a 0.68 percentage point decrease for those using tirzepatide. Both decreases were greater than the change in the placebo group (P = .008).
Change in total, basal and bolus insulin daily dose was significantly lower for adults using tirzepatide than those using semaglutide or controls. At 1 year, there was no significant difference in the change in total, basal or bolus insulin dose between the semaglutide and control groups.
“When we looked at total insulin dose per kilogram of body weight, there was a significant decrease [with tirzepatide], indicating that this went beyond just the loss of body weight and perhaps improved insulin sensitivity,” Snell-Bergeon said.
The change in BMI, body weight and HbA1c did not differ between adults receiving multiple daily insulin injections and those using an insulin pump. Snell-Bergeon said there was a trend toward greater HbA1c loss for adults receiving tirzepatide and using an insulin pump vs. semaglutide users or those using tirzepatide with multiple daily injections.
Dosing and safety
People using semaglutide began at a starting dose of 0.25 mg per week and were titrated up based on clinical guidelines. Of the group, 38 reached a maximum dose of 0.5 mg per week. For those using tirzepatide, the starting dose was 2.5 mg per week. Of the tirzepatide group, 16 reached a maximum dose of 5 mg, eight reached a maximum dose of 7.5 mg and 14 reached a maximum dose of 10 mg.
There were no reports of hospitalizations for DKA or hypoglycemia during the study. Three adults using semaglutide and one using tirzepatide discontinued the medication due to lack of response.
Snell-Bergeon said randomized controlled trials still need to be conducted to assess efficacy and safety outcomes for both medications among adults with type 1 diabetes.
Credit: healio.com
How Does Trulicity Work for Weight Loss?
Team Metabolic Health
Trulicity (dulaglutide) is FDA approved to treat Type 2 diabetes. It’s also approved to prevent heart problems in people with Type 2 diabetes and heart disease, or risk factors for heart disease.
Even though it can cause you to lose weight, Trulicity is not FDA approved for weight loss. Other medications similar to Trulicity that are FDA approved for weight loss include Wegovy (semaglutide), Saxenda (liraglutide), and Zepbound (tirzepatide).
Higher doses of Trulicity may cause more weight loss in people with Type 2 diabetes compared to lower doses.
Pix Credit: Getty Images
Living with diabetes comes with unique health challenges. Maintaining a healthy weight is one of them. Nearly 90% of U.S. adults with diabetes are considered overweight or obese. So naturally, many people with diabetes have questions about which diabetes medications can help you lose weight.
Trulicity (dulaglutide) is one potential option. It’s an FDA-approved medication for Type 2 diabetes when used along with a diabetes-friendly diet and exercise. And it’s also approved to lower the risk of heart problems in people with Type 2 diabetes and heart disease (or risk factors for heart disease). Although it’s not FDA approved specifically for weight loss, it can help in this arena as well. Here, we’ll discuss Trulicity and when it can be a tool for healthy weight loss.
How does Trulicity work for weight loss?
Trulicity is a glucagon-like peptide-1 (GLP-1) agonist. It stimulates insulin release when you eat to help control your blood glucose (sugar) levels. Trulicity isn’t FDA approved for weight loss specifically. But weight loss may be an added benefit of taking Trulicity.
GLP-1 is a type of incretin hormone. Incretins are released naturally in the body after you eat. They stimulate insulin release from your pancreas (an organ behind your stomach). This prevents blood glucose levels from rising too high.
Trulicity also slows down how quickly food travels from your stomach to your intestines. This helps you feel full sooner after eating, making you eat less. This effect helps regulate blood glucose and it can also lead to weight loss.
What does the research show about Trulicity and weight loss?
Trulicity is one of several diabetes medications that can cause weight loss. The amount of weight loss you’ll lose depends on several factors, including your Trulicity dose, how long you take it, and your starting body mass index (BMI). Generally, people tend to lose more weight with higher doses, especially if they have a higher body weight initially.
Comparing GLP-1 agonists. Several GLP-1 agonists are on the market today, and they have differences to consider.
Ozempic vs. Trulicity. Compare two common GLP-1 agonists used to treat Type 2 diabetes.
Comparing weight loss medications. Several medications are FDA-approved for weight loss, and many more are on the horizon.
In 2020, a large randomized controlled trial (the best type of study to look for cause and effect) was conducted to see how different Trulicity doses stacked up against each other. In the study, over 1,800 participants already taking metformin for Type 2 diabetes were started on Trulicity. Metformin is a common first-choice option for treating diabetes.
This study found that the amount of weight people lost, and how much their blood glucose decreased, was dose-related. People taking Trulicity 4.5 mg lost more weight (about 10 lbs) than people taking Trulicity 3 mg (about 9 pounds) or 1.5 mg (about 7 lbs) after about 9 months of treatment. Higher doses of Trulicity also decreased blood glucose more than lower doses.
The medication can be injected subcutaneously (underneath the skin) in the upper arm, thigh, or abdomen (belly). You’ll only need to inject Trulicity once a week. Be sure to use a different injection site each week. This prevents lumps from forming underneath your skin.
What’s a typical Trulicity dosage?
The starting dose of Trulicity is typically 0.75 mg once a week. You can inject Trulicity at any time of day, without regard to meals. So, pick a day and time that’s convenient for you. Just make sure you inject your dose on the same day each week.
After 4 weeks, your dose may be increased to 1.5 mg if your blood glucose is still high. Then, if your blood glucose remains high after 4 weeks, your dose may be increased by 1.5 mg every 4 weeks until your blood glucose levels are controlled. The maximum dose is 4.5 mg once a week.
Keep in mind that blood glucose goals may vary from one person to the next. So talk to your diabetes care team about what your target blood glucose range is before starting Trulicity or other diabetes medications.
Trulicity side effects
The most common Trulicity side effects are gastrointestinal (GI) side effects. People most commonly experience GI side effects within the first few weeks of starting Trulicity, such as nausea, vomiting, and diarrhea. A decreased appetite, stomach pain, and indigestion can also occur.
Less common but more serious side effects include gallbladder disease and kidney damage. In rare cases, people taking Trulicity have reported pancreatitis. And thyroid tumors have been seen in animal studies, but haven’t been confirmed in human studies.
Low blood glucose (hypoglycemia) can also occur. But it’s less common with Trulicity than some other diabetes medications, such as insulin. Hypoglycemia is typically defined as blood glucose less than 70 mg/dL. Some common signs of hypoglycemia include:
- Shakiness
- Faster heart rate
- Sweating
- Hunger
- Anxiety
- Sleepiness
- Feeling weak
- Tingling
- Confusion
- Dizziness
Check your blood glucose right away if you experience any of these symptoms. Follow instructions from your diabetes care team for how to treat hypoglycemia (such as the “15-15 Rule”), and notify them as soon as possible.
Are GI side effects worse with higher doses of Trulicity?
Not usually. You may experience GI side effects with any dose of Trulicity. But most people don’t experience worsening GI side effects as their doses are increased. In fact, side effects are most likely when you first start taking Trulicity. Severe side effects are uncommon at any dose.
Comparing GLP-1 agonists, such as Ozempic vs. Trulicity
Ozempic (semaglutide) and Trulicity are both GLP-1 agonists. They’re both injectable medications, and they’re both FDA approved to treat Type 2 diabetes and lower the risk of heart attack, stroke, and death in people with Type 2 diabetes and heart disease. What’s more, neither medication is FDA approved for weight loss, though they can both cause weight loss when used. However, two other GLP-1 agonists are FDA approved for weight loss:
Wegovy (semaglutide)
Saxenda (liraglutide)
Additionally, Zepbound (tirzepatide) is another medication that’s closely related to GLP-1 agonists and FDA approved for weight loss.
There are no studies directly comparing Trulicity to the GLP-1 inhibitors that are FDA approved for weight loss. But research has shown that Wegovy is more effective for weight loss than Saxenda. And Zepbound may cause even more weight loss than Wegovy. If you’re interested in trying any of these medications for weight loss, talk to a healthcare professional about the risks and benefits of these medications.
Good to know: The active ingredient in Ozempic (semaglutide) is also available as Rybelsus, and the main ingredient in Saxenda (liraglutide) is also available as Victoza. Tirzepatide (the ingredient in Zepbound) is also available as Mounjaro. Rybelsus, Victoza, and Mounjaro are only FDA approved for Type 2 diabetes. They’re not currently FDA approved for weight loss.
How long does it take Trulicity to work for weight loss?
How long it takes to work depends on personal factors and the Trulicity dose you’re using. The amount of weight people lose with Trulicity can vary for several reasons, including their diet and exercise routine as well as their starting weight before treatment.
In clinical studies, people taking Trulicity 4.5 mg lost about 6 lbs to 7 lbs about 3 months after starting it. By about 9 months, they’d lost about 10 pounds. Although people taking Trulicity 3 mg and Trulicity 1.5 mg doses also lost weight, they didn’t lose as much.
The bottom line
Trulicity (dulaglutide) is a glucagon-like peptide-1 (GLP-1) agonist that treats Type 2 diabetes when combined with diet and exercise. It can also be used to prevent heart problems in people with Type 2 diabetes and existing heart disease, or risk factors for heart disease.
While Trulicity isn’t FDA approved for weight loss, it’s been shown to help people lose weight, especially at higher doses (4.5 mg per week). The most common side effects are gastrointestinal-related, like nausea, vomiting, and diarrhea.
Trulicity isn’t recommended in people without Type 2 diabetes. Other GLP-1 agonists, like Wegovy (semaglutide) and Saxenda (liraglutide), are FDA approved for weight loss specifically. So is another medication that’s closely related to GLP-1 agonists called Zepbound (tirzepatide). Talk to a healthcare professional if you’re interested in trying a GLP-1 agonist for weight loss.
Credit: goodrx.com
Six common flying with food allergies myths
Team Metabolic Health
A recent review in Archives of Disease in Childhood presents common misconceptions regarding food allergies during air travel and discusses strategies to help prevent them.
Background
Food-allergic passengers feel heightened anxiety while flying due to the perceived risk of peanut or tree nut particle exposure through airplane ventilation systems. Food allergies can result in anaphylaxis, a life-threatening allergic response. Fear of severe responses lowers quality of life, particularly during holidays and travel. Dispelling myths about air travel-related food allergies could increase confidence among food-allergic individuals.
About the review
The present review discusses myths and evidence regarding in-flight food allergies and mitigation strategies based on the 2023 United Kingdom Civil Aviation Authority (CAA) report.
Common myths and evidence regarding food allergies during air travel
Myth 1: Allergic responses are more frequent on airplanes
The evidence: Research shows that individuals with food allergies are 10 to 100 times less likely to develop allergic reactions on a flight. The low frequency of allergies among food-allergic passengers may be attributed to the measures taken when flying.
Myth 2: Aerosolized food allergens are a major concern
The evidence: Allergies to aerosolized meals are infrequent, except for exposure to vapors from fish or seafood or occupational allergens such as wheat flour in baker’s asthma and seafood in fish market workers.
Myth 3: Peanut particles in ventilation systems trigger reactions
The evidence: Individuals with food allergies think peanut particles may transfer through aircraft passenger cabin ventilation systems and induce allergic responses. However, such occurrences are rare. Deshelling roasted peanuts can produce low-level but detectable peanut allergens in the air. However, aircraft ventilation systems successfully remove most nut particles in circulation. Allergies most likely result from the unintentional eating of allergen-containing food and the spread of allergen residues from seat or tray surfaces to hands, subsequently transferred to safe food ingested.
Myth 4: Nut consumption bans prevent in-flight allergies
The evidence: People think requesting passengers not to consume nuts can prevent in-flight nut allergies. However, peanut residues on seats from prior flights cause significantly more exposure than nut-eating on a current flight. Cleaning seat surfaces, tray tables, and seat-fixed entertainment systems with wet wipes before beginning flight travel is far more effective in reducing allergy risk. Nut ‘bans’ might sometimes lead to false reassurance.
Myth 5: Homemade food is safer than airline meals
The evidence: Individuals with food allergies frequently avoid airline meals and carry homemade food. However, food allergies on a flight occur after consuming homemade food and items purchased on flights, typically due to human errors in buying items that may contain allergens. Airlines frequently provide allergen-free meals if informed in advance.
Myth 6: Medical authorization is required to carry adrenaline injectors
The evidence: Individuals assume medical authorization is necessary to transport adrenaline injectors on an airplane. However, UK legislation permits individuals prescribed adrenaline autoinjectors to carry them without such restrictions.
Onboard medical tool kits rarely include autoinjectors, and cabin crew members may not always have permission to use autoinjectors. Thus, food-allergic passengers with anaphylaxis risk should carry two adrenaline injectors in cabin baggage with them when flying.
Air circulation systems for passenger cabins on commercial planes
Environmental control systems (ECS) in airplanes regulate cabin air pressure, supply, and temperature to provide passengers and cabin crew with a pleasant atmosphere. The systems assure the removal of carbon dioxide, smells, and other airborne impurities, necessitating high airflow rates throughout the cabin. Air enters the cabin from overhead distribution outlets in a regulated circular airflow pattern. The pattern causes air to circulate throughout the aircraft, limiting the spread of pollutants.
ECS delivers approximately 20 cubic feet of air per minute per passenger, resulting in a full cabin air exchange every three to four minutes. In commercial airplanes, over 50% of the air intake is recirculated air passed through high-efficiency particulate air (HEPA) filters. HEPA filters remove 99.97% of particles at 0.3 µm, including dust, vapors, and microbiological diseases. They also capture the majority of aerosolized food particles. HEPA filtration and the frequency of full cabin air exchange (15-20 times per hour) lower peanut residue in dust suspended in cabin air.
Conclusions
Based on the findings, peanut and tree nut allergies are not disseminated via airline cabin ventilation arrangements but through accidental dietary ingestion of allergens or their residues on seat surfaces.
Announcements recommending that passengers avoid nuts may not prevent in-flight responses. Cleaning sitting places with a moist wipe is an excellent method.
Airlines must have defined food allergy-related policies mentioned on their websites and routinely followed by cabin crew and ground workers.
‘Buffer zones’ in which passengers surrounding a food-allergic traveler are urged not to consume the allergen may give reassurance but pose concerns about which allergens other passengers can be asked not to ingest.
Credit: news-medical.net
Food packaging should have labels on front about health impact, says WHO
Team Metabolic Health
Packaged food and drinks should have easy-to-read nutritional information on the front of the products to help consumers make healthier choices, according to the first-ever World Health Organization draft guidelines that stopped short of recommending harsher warning labels.
Increased consumption of processed foods high in salt, sugar and fat is a key driver of a global obesity crisis, with more than a billion people living with the condition and an estimated eight million early deaths every year due to associated health problems like diabetes and heart disease, WHO data shows.

A customer shops for dairy products at a grocery store in Saint Petersburg, Russia. REUTERS/Anton Vaganov/File Photo
Yet governments have struggled to introduce policies to curb the epidemic. Currently, only 43 WHO member states have any kind of front-of-package labelling either mandatory or voluntary, the UN agency told Reuters, despite evidence showing labels can affect buying behaviour. The WHO began work on the draft guidelines, which have not been previously reported, in 2019. They aim “to support consumers in making healthier food-related decisions,” Katrin Engelhardt, a scientist in the Nutrition and Food Safety department of the WHO, told Reuters by email.
A public consultation on the guidelines closed on Oct. 11 and the finalized version will be released in early 2025.
The WHO’s guidance recommends governments implement “interpretive” labels that include nutritional information and some explanation of what that means about the healthiness of a product.
An example would be NutriScore, developed in France and used in a number of European countries, which ranks food from A (green, containing essential nutrients) to E (red, containing high levels of added salts, sugars, fats or calories).
Chile and several other countries in Latin America use a tougher system, with warnings that a food is “high in sugar”, salt or fat on the front of the package, in a black octagon that resembles a stop sign. Food labelling expert Lindsey Smith Taillie, co-director of the Global Food Research Program at the University of Chapel Hill, North Carolina, said the food industry has pushed back against warnings and favours “non-interpretive” labels, which include the nutrient information but no guide on how to understand what that means, such as those used in the United States. This week, U.S. Senator Bernie Sanders announced plans for a Senate hearing on tougher food labelling in December. While the WHO recommendation goes a step further than the industry’s preference, it “is fairly weak,” Taillie said.
Credit: Reuters
Could Weight-Loss Drugs Help Get People Back to Work?
Team Metabolic Health
The British government announced a multimillion dollar pharmaceutical partnership with Eli Lilly, including a trial that will study the impact of a weight-loss drug on work and productivity.
Around one in four adults in Britain is obese, according to estimates from the country’s National Health Service, and the problem costs the public health care system billions every year.
Now, the government says that weight-loss injections might be part of the solution, and might even help boost Britain’s productivity, which has been sluggish for years.
Studies show that people with obesity are more likely to find that ill health affects their productivity and attendance at work. On Monday, the government announced a 279 million pound (around $365 million) investment from the pharmaceutical company Eli Lilly. Among other things, the investment will help explore new ways of delivering health services to people living with obesity, and include a five-year trial of the company’s drug tirzepatide, also known as Mounjaro, which is used to treat diabetes and for weight loss.

On Monday, the British government announced a five-year trial of the weight-loss drug tirzepatide, also known as Mounjaro. Credit: George Frey/Reuters
The trial, in the Greater Manchester area in northern England, will study the effectiveness of tirzepatide in bringing about weight loss, preventing diabetes and tackling obesity-related health conditions. It will also aim to collect data on whether the drug leads to changes in participants’ employment status and sick days from work, according to a statement from the Health Innovation Network, the innovation arm of the N.H.S.
The government said that up to 3,000 people could eventually take part in the study.
Prime Minister Keir Starmer, speaking to BBC Breakfast on Tuesday, said he believed the drugs could be “very important for our economy and for health,” adding that tirzepatide “will be very helpful to people who want to lose weight, need to lose weight, very important for the economy so people can get back into work.”
Wes Streeting, Britain’s health secretary, wrote in an opinion piece in The Telegraph that the country’s “widening waistbands are also placing significant burden on our health service,” noting that illnesses linked to obesity cost the country’s health service roughly $14 billion a year.
“The long-term benefits of these drugs could be monumental in our approach to tackling obesity,” Mr. Streeting wrote. “For many people, these weight-loss jabs will be life-changing, help them get back to work and ease the demands on our N.H.S.”
But he added that “there must remain a responsibility on us all to take healthy living more seriously,” and said that the country’s health service “can’t be expected to always pick up the tab.”
Credit: The New York Times
The dark reality of melatonin behind India’s USD289 million wild chase for good sleep
Team Metabolic Health
Synopsis
Most Indians are sleep-deprived and are turning to melatonin for a better night’s rest. The global melatonin market reached USD2.15 billion in 2022, and India’s sleep aid market is projected to generate USD289 million in revenue in 2024 alone. While melatonin is often considered harmless, everything has a flipside.
We all know about ‘city that never sleeps’. Now, move over to a ‘world that never rests’. You are exhausted but can’t sleep. What do you call that feeling? According to Juhi Bajaj, a 21-year-old home tutor and devout follower of Instagram sleep coach Cayla Solomon, it’s simply “brain-fried”. Ironically, Bajaj’s WhatsApp status reads “sleeping”, though she hasn’t had a good night’s rest in months – until she caved to the trend sweeping the sleep industry: melatonin supplements.
With a purple bottle of Vicks ZZZquil gummies on her side table, Bajaj is far from alone in this quest for better sleep. The melatonin supplement market, valued at USD2.15 billion in 2022, is booming. But why is everyone suddenly so obsessed with catching ZZZs?
Blame the urban grind where time is all – ‘cruel, a thief, and a villain’. It sends people on a wild chase round the clock, trading their precious sleep for all their unfulfilled dreams.
To reclaim their forty winks, many are turning to melatonin. Once naturally produced by the body, it’s now bottled for convenience, promising to nudge sleep cycles back on track.
But is it the solution we need? Here’s what the numbers say.
In 2023, global melatonin production hit 3,500 thousand tonne. It is projected to skyrocket 134% to 8,200 thousand tonne by 2034.
And the world is wide awake, waiting for more. This is their story.
Munching on melatonin
Indians are waking up to melatonin in a big way. The market is estimated to grow at a strong CAGR of 10.4% from 2023 to 2033. In 2024 alone, India’s sleep aids market is expected to generate a solid USD289 million in revenue. And with the overall sleep industry valued at INR12,000 crore-INR14,000 crore, the demand is clearly rising.
So, what’s the top choice for sleep aids? Anything but a tablet.
Avnish Chhabria, founder of Wellbeing Nutrition, told ET Prime that global brands are already eyeing India’s growing appetite for supplements, including melatonin. Australia’s Swisse, for example, launched its SwisseMe Melatonin Gummies in India in 2022, and has quickly caught on.
But Indian brands like Wellbeing Nutrition aren’t backing down. Their plant-based melatonin sleep melts (available in 5mg or 10mg) are designed to promote relaxation and better sleep.
What’s their recipe? Chhabria explains the company’s ‘Oral Thin Strip’ technology allows melatonin to be delivered directly through the buccal layer of the mouth, ensuring 100% absorption into the bloodstream bypassing the gut.
When it comes to sales, quick-commerce platforms like Blinkit and Zepto are Chhabria’s go-to picks. With the company’s ARR (annual recurring revenue) surging from INR100 crore to a projected INR240 crore this year, it is evident that sleep-deprived Indians are driving this growth.
An e-mail sent to P&G, the leader in the segment with Vicks commanding 60% of the market share, remained unanswered until the time of publishing this article.
Manju Sharma, a 58-year-old homemaker in Delhi’s Sarita Vihar and single parent to a software engineer working odd hours, has found solace in a melatonin spray to catch some sleep between her son’s US-timed shifts. “It’s been three months since I started using melatonin spray [Carbamide Forte Melatonin 5mg]. Just two-three sprays and I am asleep in 15-20 minutes,” she shares.
But does it guarantee a morning as fresh as a daisy? Not quite.
The dark side
While the spray initially helped Sharma achieve restful sleep, she gradually began to feel heavy-headed upon waking up. Does she blame the product? Of course not. “Perhaps it is the milkman buzzing the doorbell or the barking dogs,” she muses.
Meanwhile, an ENT clinic, just a few blocks away, reported a case of acute shortness of breath in a patient who combined her bronchodilator with the melatonin spray. The patient, a young lawyer, was promptly transferred to the nearby Apollo Hospital where her condition improved, suggesting that these sprays may not be suitable for individuals with lung diseases – at least in some cases.
Does research back this up?
The European Medical Journal has found evidence indicating that melatonin use can exacerbate night-time asthma symptoms by constricting airways. This is due to its activation of the melatonin MT2 receptor, which influences the circadian rhythm and can counteract the effects of bronchodilators, particularly at high dosages.
So, is a moderate amount safe for long-term use?
Neurologists say no.
Here’s why.
As we age, our body’s melatonin levels naturally drop, which can lead to poor sleep quality or even insomnia. While melatonin supplements are widely available and popular for treating sleep issues, they are not a long-term solution. “Melatonin is most effective for temporary problems like jet lag or shift work disorder,” explains Praveen Gupta, principal director and head of neurology at Fortis Hospital, Gurugram. Taking it without a proper diagnosis won’t address the underlying sleep disorder.
The challenge also lies in figuring out the right dosage. With so many forms – patches, sprays, gummies, syrups, melts – each featuring different absorption rates, self-dosing can get a bit tricky. Unregulated use can cause side effects like dizziness, headaches, nightmares, palpitations, and even brain fog.
Without medical supervision, overdosing is a real risk. Take 27-year-old Niharika Basu, a BPO employee in Gurugram. Struggling with sleep due to irregular work hours, she tried melatonin gummies on a friend’s recommendation. Assuming more would be better, she took two 5mg gummies – unaware the typical starting dosage is just 1mg-3mg. A few hours later, she felt drowsy, disoriented, and nauseous – symptoms indicative of an overdose.
For those with conditions like epilepsy or heart issues, melatonin can be especially risky. “Melatonin can be helpful,” says Delhi-based nutritionist Divya Gandhi, “but overuse can lead to toxicity, and long-term use may disrupt neurotransmitters, triggering anxiety and worsening sleep once stopped.”
It is important to remember that, even though it is non-habit forming, melatonin is still a drug that should be used judiciously,” Gandhi adds.
Despite its availability over the counter (OTC) in India, melatonin is tightly regulated in countries like the UK, the EU, Japan, and Australia, where it is available only by prescription.
Doctors in India express concerns about dosages as high as 20mg being available OTC, warning that it should be used cautiously.
No child’s play
Sure, the adage goes, ‘Every child you encounter is a divine appointment’ but in no way does it imply parents can surrogate for a pediatrician and meet those appointments.
If the child is having trouble sleeping or is too active during the night, the young millennial parents are self-administering melatonin gummies to their children – regardless of whether it’s suitable for their age-group.
“The easy access to melatonin gummies can lead to self-medication, skipping proper diagnosis, and exposing children to unknown risks,” warns Gupta. Prolonged use, especially in young children, could stall brain development, leaving their minds dull.
In some cases, long-term melatonin use in children has been linked to delayed puberty, though this remains debated.
“Children naturally produce enough melatonin. Giving them supplements can cause dependency and lead to harmful effects,” cautions Gandhi. “Unfortunately, many parents turn to Google and Instagram for health advice instead of consulting professionals. It’s worrying.”
But does this stop parents? Not really.
On X (formerly Twitter), countless parents rave about the effects of melatonin on their kids, especially the US version of Vicks PURE Zzzs Kidz Melatonin Gummies. Amazon reviews hail it as a trusted household product.
A 2022 study highlighted the surge of 150% in melatonin sales between 2016 and 2020, leading to increased access among children.
As a result of this, in the US, from 2019 to 2022, Center for Disease Control and Prevention (CDC) reported 11,000 emergency department visits due to unsupervised melatonin ingestion by children aged five and under, often involving flavoured products.
If that’s not enough to raise an alarm, the US poison-control centre reports about melatonin ingestion by individuals aged 19 and under rose from 8,337 in 2012 to 52,563 in 2021, with hospitalisations and serious outcomes also increasing, particularly among teenagers and children aged 5 and below.
Though India lacks kid-specific melatonin supplements, parents aren’t hesitating to let their children take a bite of their gummies or use a sleep melt.
“They would be better off with fresh cherries, soaked walnuts, or bananas,” Gandhi suggests, noting that these foods can naturally boost the body’s melatonin production.
It’s all psychological
A Delhi-based clinical psychologist revealed to ET Prime that the long-term use of supplements can be traced back to classical conditioning. Users often develop habitual behaviour, regardless of whether the product has potential for physiological dependence.
This behaviour is fuelled by psychological trust and reliance on the supplement, creating a placebo-like effect where users feel the supplement is essential for their well-being.
This creates a psychological dependence, where the perceived need for the supplement becomes deeply entrenched in daily routines, making it tough to quit without feeling anxious or distressed. Moreover, the ritualistic aspect of taking supplements can offer a sense of control and security, further strengthening the behaviour.
And when you do try to stop, withdrawal symptoms may follow.
One user, who turned to melatonin gummies for exhaustion and anxiety-induced insomnia, described her withdrawal: “What promised to be a sleep solution quickly turned into a headache – literally.” She faced persistent headaches, mood swings, and anxiety that disrupted her daily life for days.
This could be partly psychological, but it might also be the body’s physiological rebound after discontinuing prolonged melatonin use.
“Even harmless things, when overused or abused, can become harmful,” says Gupta.
The jury is still out
In India, a study conducted back in 2015 found that 93% of Indians are sleep-deprived, and 34% have sleep apnea. We have surely come a long way, but here’s a quick reminder before we call it a wrap – Melatonin supplements do work – but on all? The same way? Nay-nay.
As we took leave of Bajaj, the home tutor cited earlier, her phone buzzed with a new Instagram notification from Solomon, her favourite sleep coach. But this wasn’t just any notification – it was a reminder for her melatonin gummy, a signal that sleep in the modern world is as much about routine as it is about rest.
Because eventually, for many, it’s not just about finding sleep – it’s about managing it.
And so, the cycle continues.
(Graphics by Sadhana Saxena)
Credit: ET World
