The great pharmaceutical-academic merger
Team Metabolic Health
As drug companies fret over their finances, they are increasingly partnering with universities to help with early-stage research
Pharmaceutical companies are often lambasted for rising drug costs. For example, the price of new drugs entering the US market in 2023 was 35% higher than in 2022. According to an analysis from Reuters, part of the increase is due to a move to develop therapies for rare diseases: because fewer people have those condition, drugmakers push up the per-dose price to recover their costs. But the cost of developing drugs for more common diseases, including cancers, is also rising rapidly.
In 2019, pharmaceutical companies spent $83 billion dollars on research and development. After accounting for inflation, that’s roughly 10 times what the industry spent in the 1980s, according to the US Congressional Budget Office. A 2024 study showed that the share of sales revenue devoted to research spending rose from 12% in 2008 to 18% in 2019, and drugmakers are beginning to feel the pinch.
In addition to rising research costs, several blockbuster drugs will soon be old enough to be reclassified as generic, meaning their developers are set to lose their status as the exclusive manufacturer, says Magid Abou-Gharbia, founding director of the Moulder Center for Drug Discovery Research at Temple University. “When that happens, you can kiss the money goodbye,” he says.
Drug companies are increasingly looking to academics in a bid to mitigate some of these financial burdens. This often involves university researchers doing early-stage drug discovery before pharmaceutical companies take over to push a novel compound through clinical trials and get it to market. “This trend is not entirely new,” says Karl-Heinz Altmann, a synthetic organic and medicinal chemist at the Swiss Federal Institute of Technology (ETH), Zurich. “But it does have momentum now.”
Financial booster
In the life sciences, corporations have been scaling back their in-house research since the 1980s. According to the Nature Index, which tracks the output of 82 scientific journals, research partnerships between companies and academic institutions more than doubled between 2012 and 2016.
A 2022 report from the Association of the British Pharmaceutical Industry found 2,687 links between the UK pharmaceutical industry and academia in 2022, compared with 1,134 in 2003. In other words, collaborative work with academics is making up a larger share of research by private companies, including drugmakers.
“Pharmaceutical companies are moving to work more with academic centers to reduce their risk exposure,” says Kelly Chibale, an organic chemist and director at the University of Cape Town Drug Discovery and Development Centre. “It’s not a coincidence that Boston in the US or Oxford and Cambridge in the UK have so many major pharmaceutical companies. They’re based there because that’s where the academics that they want to collaborate with are.”
From pharma’s perspective, the proof-of-concept stages of drug development are laden with the risk of failure—something their accountants are keen to avoid. By comparison, academia is relatively unbothered by failure if lessons can be learned and—crucially—if papers can still be published. But even with spinout and start-up companies, universities lack the infrastructure to progress a novel compound much further than proof of concept. Clinical trials are just too expensive. If done right, collaborations between the two worlds can be mutually beneficial.
Along with the shift of drug discovery to the academic world, larger numbers of researchers are moving from pharmaceutical companies into academic roles.
For instance, Altman worked at Novartis until 2003, when he moved to ETH Zurich. “I was offered the job. I didn’t seek it out,” he recalls. “It was a difficult decision to go from a well-established environment where you know people to a situation where you have to start from scratch. It’s not like you’re a professor moving from one university to another where you can take your research with you. What I did at Novartis stayed there. All I had was a lab and a budget to develop ideas.”
The move involved a number of serious considerations—starting with the drop in salary. “I don’t think anything that a head of research can earn in industry would ever be matched by a university,” Altman says. “I would probably make twice as much money if I’d stayed in industry.” But he says the freedom to choose a research path was worth the sacrifice in salary.
Altman’s move into academe is part of a wider trend within drug development research as more people move back and forth between industry and universities. “Industry is stepping out of the very early stages because it’s becoming more and more expensive,” says Peter Nussbaumer, managing director at the Lead Discovery Center in Dortmund, Germany, a translational drug research company founded by the Max Planck Society’s technology transfer arm, which collaborates with academic partners.
As more early-stage research moves from industry to academia, so too do people, Nussbaumer says. And academic drug discovery centers have become a destination for them.
Those who dare, win
In 2008, Abou-Gharbia left his job as a senior vice president at Wyeth Research—which was later acquired by Pfizer—to become a professor of pharmaceutical sciences at Temple University. As part of his recruitment, Abou-Gharbia was tasked with kick-starting drug discovery research there. The concept was something of a novelty at the time, he recalls. “There were only a few drug discovery centers in universities,” he says. Now, according to a 2017 study authored by Abou-Gharbia, there are close to 100 such centers in the US alone.
A growing trend
A year after starting at Temple, Abou-Gharbia was awarded a $1 million stimulus grant from the National Institutes of Health. He then wrote a pitch to establish a drug discovery center, which would include cutting-edge technologies used by the pharmaceutical industry. The university’s leadership approved the proposal and backed it with about $8.2 million, which allowed the center to recruit researchers and build laboratories.
The Moulder Center is celebrating its 15th anniversary this year. Since its founding, the center has received more than $35 million in outside support—enough to enable its staff to publish more than 180 papers in peer-reviewed journals and file more than 30 patents. Moulder has also created four spin-off companies and trained many future researchers in modern drug discovery and development. “Many universities ask me how to establish similar centers and I tell them you need university support and money,” Abou-Gharbia says.
You also need industry researchers to be readily accepted into academic roles, as Abou-Gharbia was. Such a career move used to be hard to pull off. Though being poached by industry was a well-trodden path for academics, going in the other direction was relatively rare until just a couple of decades ago. This is still the case in much of the EU, according to Nussbaumer. “It’s much easier to go back and forth in the UK and US,” he says. “Not so much in mainland Europe.”
Altman agrees but says Germany and other EU countries are beginning to catch up. “It’s starting to become a bit more relaxed,” he says.
Universities used to be rigid and highly particular about what kind of experience qualified a person for the job, Nussbaumer says. And there was a question of values: Are you in it for the money or the science? But those boundaries have become less defined in recent years, thanks in part to the promise that researchers can achieve scientific progress and make money by building small companies on the back of their research with the hope of attracting the interest of a larger drug developer.
Fernando Albericio, an organic chemist at the University of KwaZulu-Natal, has noticed that this way of thinking has also started to inform the career goals of students and young researchers. “In the past, a PhD student typically wanted to work in academia for life,” he says. These days, their ambition more often is to start a company.
“The number of spin-off companies is rising rapidly, and they have a sense of being the bridge between academia and pharmaceutical companies,” Albericio says. Drug discovery centers and spinouts enable the academic scientist to carry on their work with one foot in each door.
Drugmakers’ courtship of academic scientists is about more than quelling their financial fears. “It’s part of it, sure. But it’s also that drug discovery has gotten harder because the easier drugs to discover have already been discovered,” says preclinical pharmacologist Charles Hart, who earlier this year became codirector of the Small Molecule Discovery Center at the University of California, San Francisco (UCSF), after 30 years in biotech. “We need new drugs in cancers and new diseases like COVID-19 and other infectious agents, which is just really hard.” Hart says that industry also wants and needs access to the cutting-edge know-how that academic researchers possess.
University-based drug discovery centers and their start-up firms offer pharmaceutical companies the opportunity to use the findings and results that academic experiments have yielded. Sometimes firms exploit those data to further the research that they’re are already doing; other times they want to get a leg up on a research program into a new field in which they lack expertise. Companies may also want to buy up specific compounds and therapies that have shown promise in early experiments.
In addition, technological advances in recent years have opened up new avenues of exploration that companies want access to. Whether it’s artificial intelligence, sophisticated cellular techniques, or gene therapies, drugmakers are looking for help in exploiting these developments. “Both biology and chemistry, as fields, have widened a lot in recent years,” says Michelle Arkin, a chemical biologist who works with Hart as codirector of the Small Molecule Discovery Center at UCSF. “There’s a real enthusiasm in the pharma companies to take advantage of this.”
This sentiment is echoed by Carsten Schultz, a social scientist at Christian Albrechts University of Kiel whose research has investigated the effects of university-industry collaborations on research and development performance. “Even the big pharmaceutical companies need to leave old fields of activity and engage in new fields like biotechnology and cell therapies,” he says. “Pharma needs to invest in these new technologies in the medium term, but they really need academics to get ahead on the knowledge.”
Who benefits?
An optimist would say these partnerships are a way for both sectors to bring their strengths to bear: academics get more funding, pharmaceutical companies get reduced risk and more expertise, and patients get more drugs. The skeptic would say that big pharma is offloading the risk burden onto academic researchers—and the public agencies that fund them—while enjoying the fruits of their labor when things do work out.
“If you consider this from the societal part of things, the question is who takes the financial burden,” Schultz says. “Whether a university or researcher makes money depends on the system. In Germany we still have a very traditional academic system. Legally, whatever happens at the university belongs to the university.” That makes spinout companies a challenge to establish, although Schulz says there are efforts to improve this.
Even if a university administration is open to the idea of its scientists starting a business, each agreement for an academic working with a pharmaceutical company is unique. “The devil is in the details,” Arkin says. “It can be exploitative, but it can be mutually beneficial.” It’s important that scientists on both sides openly discuss what they want to get from the collaboration before any draft agreement is drawn up, she adds. “As soon as the contract writers become involved, it will be more adversarial, but if scientists on either side generally have a shared vision, that’s a good start.”
Not all agreements are created equal, and academic researchers can have various degrees of engagement. “We’ve done many collaborations where we’re so involved that we go to all [the company] team meetings, and we discuss everything with them,” Arkin says. “And then sometimes we just get paid for what we do as contractors and never really find out exactly what they do with our results. Sometimes they keep the drug target a secret from us. It just makes supplementary income for our research.”
There’s no right or wrong way to do it, but researchers should just think about what they want before signing, according to Arkin. “There’s cheap money and expensive money,” she says. “Don’t get involved in the expensive money that sees you doing things you don’t want to do or aren’t interested in.”
Why drug development has become so expensive
Drugs are getting more expensive for patients, insurers, and governments. Critics say that is down to a desire for bigger profits, but costs for pharma companies are also increasing.
A 2020 study comparing the revenues of 35 large pharmaceutical companies with those of 357 other large firms in the S&P Index showed that the former had an average profitability rate of 13.8% compared with just 7.7% for the latter.
But it’s also true that progressing a new drug from the initial stages of molecule discovery through packaging and product placement has never been more expensive. Studies estimate that the average research and development costs for a new drug range from $314 million to $2.8 billion, depending on factors that include target disease and failure rate, and whether the drug has an entirely new unique mode of action or not. Drug companies argue that these rising costs are cutting into their margins.
You can see evidence of that in the number of research site closures, says Magid Abou-Gharbia, founding director of Temple University’s Moulder Center for Drug Discovery Research. Staff layoffs accompany this trend. Bristol Myers Squibb expects to cut 2,200 jobs by year-end. Novartis laid off 29 employees in San Diego and expects to drop a further 100 jobs as it winds down its research site there. Takeda cut 440 workers from its staff in July, and the list goes on.
Recent years have also seen a flurry of corporate restructuring, which can mask the industry consolidation, Abou-Gharbia says. “When I started out there were 50-plus big pharma companies, but through mergers and acquisitions, it’s gone down to about 10. They call it synergy, but it’s really downsizing.”
There are many other interlinked factors behind increasing costs. Inflationary pressures are certainly one, as is cutting-edge science. Gene and cell therapies, for example, require expensive technology and equipment that pharmaceutical companies don’t necessarily have—so as science advances, so do the overhead costs.
Growing red tape is another contributor. “Regulatory agencies like the US Food and Drug Administration and [the European Medicines Agency] are asking for more and more paperwork and hurdles to get approval,” says Fernando Albericio, a research professor and organic chemist at the University of KwaZulu-Natal.
This bureaucratic burden means clinical trials take longer and cost more. In 2018, the Tufts Center for the Study of Drug Development investigated the amount of time drugs spend in clinical trials before an approval is granted. Between 2008 and 2013, the average was 83 months; that figure rose to 90 months between 2014 and 2018.
The good news for pharmaceutical companies is that data from a 2024 Deloitte analysis give reasons to believe the industry is turning a corner. The report measures the return on investment from the research efforts of 20 large biopharma companies. The return on investment last year was 4.1%, a significant bump from the all-time low of 1.2% the year before. The hope is that investments in new technologies such as artificial intelligence will start to yield results and sustain this recovery.
Credit: cen.acs.org
World First: Stem Cells Reverse Type 1 Diabetes in Clinical Trial
Team Metabolic Health
Most people with type 1 diabetes cannot reverse their autoimmune disease or put it into spontaneous remission – all they can do is manage their blood sugar levels with insulin, a healthy diet, and regular exercise.
Now, the successful treatment of the condition in a young woman in China has brought the possibility of a universal cure tantalizingly close.
In June 2023, doctors injected the equivalent of roughly 1.5 million insulin-producing cells into the patient’s abdominal muscles. The community of cells was carefully reprogrammed from her own stem cells.
Two and a half months later, the woman’s lifelong dependence on injected insulin came to an end – completely reversing her long-term, hard-to-control diabetes.
More than four months after the transplantation, her body was producing enough insulin on its own to keep her in a safe blood glucose range for more than 98 percent of the day.
If this one patient can keep producing insulin naturally in the coming years, she could one day be declared ‘cured’ – the first successful case of its kind in the scientific literature.
“That’s remarkable,” diabetes researcher Daisuke Yabe, who was not involved in the research, told Nature reporter Smriti Mallapaty.
“If this is applicable to other patients, it’s going to be wonderful.”
Researchers in China are already planning to open up their trial to new patients.
Type 1 diabetes occurs when the body’s immune system attacks clusters of cells in the pancreas that produce insulin, called islets.
Transplanting islets or an entire pancreas from a donor to a patient with type 1 diabetes can prove curative in some selective cases, but it is an extreme and potentially dangerous option, and there are too few donors to make it accessible for the millions of those with this autoimmune disease worldwide.
For over two decades now, scientists have tried to coax cells from fully-developed adult tissue types back into a blank state known as an induced pluripotent stem cell, and in turn, transform them into insulin-producing cells.
Figuring out how to do that with accuracy, however, is tricky work. The final product doesn’t always match real pancreatic islets.
Researchers in China have taken a new route that they say allows them greater control. Instead of introducing proteins to the stem cells, which trigger certain gene expressions, reprogramming the adult tissues into the blank state, the team has engineered induced pluripotent stem cells using small molecules.
After testing the technique in mice and non-human primates with success and safety, the team of researchers got their approval for a human clinical trial. The trial is ongoing, and three people are currently enrolled.
One of those patients is a 26-year-old woman, who was diagnosed with type 1 diabetes at age 14, and her results from one year in the trial have now been published.
Previously, this patient had already had a pancreas transplant for severe hypoglycemia, but the organ had to be removed due to “severe thrombotic complications”.
So far, her stem cell transplant seems to be working better, alongside her immunosuppressive drugs.
The findings join several other recent clinical trials that suggest further studies on stem cell transplantations are warranted.
In a trial in the US, for instance, a dozen patients with type 1 diabetes were injected with islets, created from donated stem cells. The group was also treated with immunosuppressants. All 12 participants began producing insulin naturally when glucose entered their bloodstream, according to preliminary results.
“Overall,” write the researchers in China, “the findings support further clinical studies in this direction and mark a step forward in achieving the potential of personalized cell therapy… to treat disease.”
The study was published in Cell.
Credit: sciencealert.com
Gene-editing drugs are moving from lab to clinic at lightning speed
Team Metabolic Health
One autumn day in 2020 Patrick Doherty was walking his dog up a steep mountain in County Donegal, Ireland, when he noticed he was, unusually for him, running out of breath. The eventual diagnosis was terrifying: amyloidosis, a rare genetic disease that caused a protein, amyloid, to build up in his organs and tissues. The prognosis was even worse: it would cause him years of pain until it finally killed him. In the face of such terrible fortune, though, Mr Doherty had a stroke of luck. He was able to join a trial of a new medical therapy and, with just a single injection, was apparently cured. Now, he continues to walk his dog up that steep mountain in County Donegal every week.
Scientists have already used gene editing to improve the vision of people with an inherited condition that causes blindness. Image: Pixabay
The treatment edited Mr Doherty’s genes using CRISPR-Cas9, a technology that has moved from lab to clinic at lightning speed. Scientists have already used gene editing to improve the vision of people with an inherited condition that causes blindness. They also appear able to cure sickle-cell disease with it, and to restore hearing in deaf mice. This new class of medicines will gather pace in the coming year, tackling cardiovascular disease and cancer. A new generation of more precise and efficient gene-editing tools is also undergoing trials.
CRISPR-Cas9 acts like a pair of molecular scissors that cuts DNA at a precise location. A piece of RNA (a single-stranded version of DNA) attached to the medicine guides the cutting enzyme, Cas9. Once DNA is cut, the cell’s natural repair mechanisms swing into action. Gene-editing medicines commandeer those natural cellular systems and end up replacing an existing (problematic) segment of code with a new (corrected) sequence.
The speed of innovation has been impressive. CRISPR-Cas9 was discovered in the lab in 2012 and just three years later eGenesis, a biotech firm in Cambridge, Massachusetts, had used it to edit pig embryos to create organs more suitable for transplantation into humans. By 2016 a CRISPR-Cas9 therapy was approved for testing in patients with cancer, albeit on immune cells that had been removed from the body, edited to help these cells fight the cancer better, and then returned.
The following year, Vertex and Crispr Therapeutics, pharmaceutical companies based in Boston, Massachusetts, and Zug, Switzerland, said they would co-develop a treatment named CTX001, a treatment for two disorders: sickle-cell disease and beta thalassemia. Both are caused by genetic faults in the instructions for making haemoglobin, a protein that helps red blood cells carry oxygen.
CTX001, known today as Casgevy (exagamglogene autotemcel), arrived on the market in November 2023, priced at $2.2m for a one-time treatment. It involves collecting blood stem cells from a patient, editing a gene within them to restart the production of a type of haemoglobin that is usually produced only when a baby is in the womb, and re-injecting those stem cells. The patient is then capable of creating enough healthy red blood cells to treat the symptoms of their blood disorders.
As good as it is, CRISPR-Cas9 has limitations. The RNA guide molecule can sometimes be imprecise, leading to unintended cuts to a patient’s DNA. Moreover, because the tool breaks both strands in a DNA helix, the subsequent repair can also introduce unwanted insertions or deletions. Damage to genetic information like this could eventually lead to cancer or disrupt cellular function in other ways.
Updates to the technology are thus in the works. CRISPR-Cas9 nickases, for example, are enzymes that cut only one strand of the DNA double helix. To make genetic changes, nickases therefore need to be used in pairs, meaning less risk of off-target effects. It is unlikely that both nickases in an edit would bind incorrectly to the same section of DNA. Another method, “base editing”, can chemically change a single letter of a DNA’s sequence into another without the need for cuts.
Some of these techniques are already in the clinic. In 2022 a patient with familial hypercholesterolaemia was given an infusion of a base-editing treatment as part of a trial. The disorder, which affects one in 250 people, results in reduced clearance of bad cholesterol from the blood. The treatment, VERVE-101, made by Verve Therapeutics, turns off the PCSK9 gene in the liver by making a single-letter change in the DNA (from A to G).
Beam Therapeutics, based in Cambridge, Massachusetts, is using base editing to make therapies for a range of conditions. These include making four DNA-letter changes to immune cells so that they are better able to attack leukaemia, as well as a product that works for the same diseases as Casgevy. The company reckons its base-editing drug will work better than CRISPR-Cas9 and deliver higher levels of haemoglobin. Data from early trials of base-editing technology in patients are expected in the second half of this year.
At the clinical frontier is “prime editing”, which uses a Cas9 nickase along with a specially designed RNA guide that not only locates the correct region of DNA, but also carries a template of the desired change. Also attached to the CRISPR protein is an enzyme called reverse transcriptase. This reads the RNA template and synthesises the correct DNA sequence at the location of the nicked site, giving a precisely edited gene.
In April David Liu, a molecular biologist at Harvard University, posted on X that the first trial to use prime editing in a patient had been approved only four and a half years after his lab had published the first paper on the technology. Prime Medicine, a biotech firm in Cambridge, Massachusetts, has already begun clinical trials of its drug PM359 for the treatment of chronic granulomatous disease—a life-threatening condition that affects the blood’s ability to destroy infections.
Being able to change larger pieces of the genome, as is the case with prime editing, makes it possible to treat diseases where errors stretch over a long distance, like Huntington’s disease. But it could also help with the tricky economics of treating rare diseases. Instead of making a medicine that treats a single mutation to a gene, it would be possible to fix many types of mutation with one correction. The flexibility of the technology means that, in theory, prime editing could correct almost 90% of disease-causing genetic variations.
The technological progress in gene-editing tools has not stopped. Yet another method, known as “bridge RNA”, details of which were published in Nature in June, uses a form of guide RNA that recognises two stretches of DNA—the target site and the new gene that is to be inserted. This new technique allows large stretches of DNA to be added, removed or inverted.
All these new technologies face technical and safety hurdles in the years ahead. A big question is how to deliver therapies to the right place in the body. Blood cells, cancers, the retina and the liver are all easy to reach and edit. The brain and lungs are more difficult. One solution to the delivery problem, proposed by Aera Therapeutics of Cambridge, Massachusetts, is a capsid, a nanoparticle with a protein shell. Based on human proteins, these nanoparticles could be targeted to different tissues while also not provoking a strong response from the body’s immune system.
But perhaps the biggest challenge will be economic. So far, the new generation of genomic medicines have been eye-wateringly expensive—a shot of Hemgenix, a haemophilia B gene-therapy, costs $3.5m, around a million dollars more than Casgevy. Firms believe they can charge high prices not only because of the costs of developing and making the drugs, but because they offer potentially lifelong benefits (although the durability of these treatments remains to be proved).
There are reasons to think costs might come down in time. Treating diseases that affect larger patient groups, such as heart disease, would help reduce costs. Ultimately, many believe gene-editing tools will evolve into “platforms”, where the core technology would remain unchanged and only the specific instructions for changing genes would be tweaked for new diseases. This would reduce the need for clinical trials for every new drug. Until that happens, though, firms may be forced to drop even promising treatments because of market conditions. Yet gene editing is moving so fast that it seems only a question of when, not if, these new medicines will overcome their difficulties.
© 2024, The Economist Newspaper Limited. All rights reserved. From The Economist, published under licence. The original content can be found on www.economist.com
Credit: Live Mint
Weight loss and diabetes – Know each and everything
Team Metabolic Health
Weight is a sensitive issue for many people and getting to an ideal, healthy weight is easier said than done. But when you have diabetes, there are huge benefits to losing weight if you’re carrying extra weight.
You’ll have more energy and you’ll reduce your risk of serious complications like heart disease and stroke. Losing weight can help with your diabetes control too. And if you have type 2 diabetes, losing weight could even mean going into diabetes remission.
But millions of people with diabetes find keeping to a healthy weight a huge struggle. You’re not alone in this, there’s support out there to help – a good first step is to ask your healthcare team for help and advice.
Around 60% of people with type 1 diabetes and around 85% of people with type 2 diabetes are carrying extra weight or are living with obesity.
Benefits of losing extra weight
There are so many benefits to losing extra weight – both physically and emotionally.
Extra weight around your waist means fat can build up around your organs, like your liver and pancreas. This can cause something called insulin resistance. So losing this weight could help the insulin you produce or the insulin you inject work properly.
And as you start to lose weight and get more active, you and your healthcare team may need to look at your medication, especially if you treat your diabetes with insulin or sulphonylurea. This might mean reducing the dose or making other adjustments, but talk to your healthcare team about it. For some people, needing fewer diabetes medications is a great motivation for losing weight.
Although getting type 1 diabetes has nothing to do with weight, losing any extra weight will help you reduce your risk of complications and could mean injecting less insulin.
And if you have type 2 diabetes, losing around 5% of your body weight can have real benefits for your health. If you have obesity, you are more likely to put your diabetes into remission if you lose a larger amount of weight, 15kg (or 2 stone 5lbs), as quickly and safely as possible following your diagnosis. This could mean coming off your diabetes medication completely – a life-changing possibility. This is even more likely if you lose the weight nearer to your diagnosis and quickly. It’s a myth that losing weight slowly is better for you.
Most people say they also feel better in their mood, have more energy and sleep better.
We’ve got lots of information to help you maintain a healthy weight too, to help keep you on track and prevent putting weight back on.
“We know that losing even 5% of your weight helps improve blood pressure and cholesterol levels. This can have a big impact on your overall health and go a long way to reducing your risk of serious complications, like heart disease and stroke.”
Douglas Twenefour, our Deputy Head of Care and dietitian
What’s a healthy weight to aim for?
Before you get started, you need to know what a healthy weight is and what numbers you’re aiming for. This is about working out your Body Mass Index (BMI) and your waist size.
Know your weight
Research shows that the more weight you lose, the greater the health benefits, but even losing just 5% of extra weight will improve your health.
BMI uses your height and weight to work out if you’re a healthy weight. It doesn’t look at how much fat you have around the middle, so that’s why you need to measure your waist too. You can work your BMI out for yourself using this NHS tool – it will show you your target range.
For many people living with obesity, aiming for a healthy BMI may not be realistic.
Know your waist size
- A healthy waist size depends on your gender and ethnicity. It should be:
- less than 80cm (31.5in) for all women
- less than 94cm (37in) for most men
- less than 90cm (35in) for South Asian men.
- Here’s our community champion Rohit to show you how to measure your waist.
Can diabetes cause weight gain?
If you have type 1 diabetes, when you start taking insulin, you might start to put on weight. There are lots of reasons for this, like how much insulin you take, your diet and the type of insulin you’re taking.
Insulin is a growth hormone, and any growth hormone you take will mean putting on more weight. When you’re diagnosed with diabetes it’s also likely that you lost a lot of weight in a short space of time, as this is one of the symptoms, and the weight gain is part of the recovery.
The type of insulin you take can affect your weight in different ways. We’ve got more information about the different types and how they can affect your weight.
If you’re worried about putting on weight, or you’d like some help losing weight, then we’re here to help.
Diabetes diet plans to lose weight
- You may have heard that diabetes can be controlled by diet. There is no such thing as a special diet exclusively for people with diabetes. There are a lot of different ways to lose weight – but there’s no one-size-fits-all diet.
- It starts with finding a way to eat fewer calories than you need.
- A calorie (or kcal) is a unit of energy, which is in the food and drink we consume. Your body uses energy for everything we do – from breathing and sleeping to exercising. When you eat, you’re replacing the energy you’ve used, which helps you to maintain a healthy weight.
- As a general guide, government recommendations are that men need around 2,500kcal a day to maintain a healthy weight, and women need around 2,000kcal a day. But most people need different amounts of calories based on how their bodies work, how active they are and any weight management goals.
We’ve put together some 7-day meal plans to help you lose weight. They’re all clinically approved, nutritionally balanced, calorie and carb counted, and can help if you want to lose weight:
- Low-carb diet plan
- Mediterranean diet plan
- Lower-calorie diet plans, like 1,200 or 1,500 calories a day
- Evidence shows that the best approach is the one that you’re likely to stick to. So the key is to find a plan that you enjoy and fits in with the rest of your life. Everyone’s different and what works for some may not for others.
Low-calorie and very low-calorie diets
A low-calorie diet is made up of between 800 to 1200 calories a day – our DiRECT study used a low-calorie diet of around 850 calories a day to see if type 2 diabetes could be put in to remission. But DiRECT is not a diet. It’s a weight-management programme, delivered in GP practices in some areas of the country.
Then there’s a very low-calorie diet, which means having less than 800 calories a day.
We haven’t created low or very-low calorie meal plans as these could be challenging for most people to make themselves at home. Most people who follow these diets use special meal replacement products, likes soups and shakes, which are nutritionally complete. If you chose to try a low-calorie diet like the one in DiRECT, speak to your GP or nurse first, especially if you use medications like insulin.
Other diets
A low GI diet can help you manage your blood sugar levels, but the evidence for people with diabetes losing weight is not very strong.
There are other popular diets, like intermittent fasting (such as the 5:2 diet) and the Paleo diet. Unfortunately there isn’t enough strong evidence to say these are effective for weight loss in people with diabetes either.
Commercial weight-loss programmes
Some people feel that they need more support and choose to join a commercial weight-loss programme. These usually involve calorie-controlled eating plans or meal replacements, like milkshakes or bars.
It’s really important to ask lots of questions about these programmes, so you’ve got all the evidence and information you need to make an informed decision. Here are some ideas:
- Has a healthcare professional been involved?
- Does the programme offer advice on your diabetes (especially if you’re at risk of hypos)?
- Are you getting all the nutrition you need from this programme?
Does the programme give support and education?
Whether you choose to try one of our meal plans, or another type of diet, it’s really important that you talk it through with your diabetes team first. Starting a new diet will affect your medication or blood sugar levels, so you need their knowledge and support.
Weight-loss planner
“I keep a daily diary and log my weight and activity. It keeps me accountable and focused.”
Edward Morrison
You can download My weight-loss planner (PDF, 534KB) to set goals and track your progress. By putting a plan in place and noting down your progress, you’ll be able to see the positive changes you’re making.
Your feelings about food
The emotional part of trying to lose weight is important and can often be overlooked.
Do you feel guilty when you eat a treat? Do you eat more when you’re upset? Do you feel dejected if you can’t see progress straight away?
These are really common feelings and tackling them can help you on the road to a healthier lifestyle and a healthy weight.
Find out more about your feelings about food and diabetes.
Connect with others and share tips in our online forum – we’ve made a board especially for people who are looking to lose weight.
Exercise and being active for weight loss
Regular exercise or physical activity has many health benefits and will help you in your weight loss journey. We’ve got more information about how much activity you should be doing and different ways to get active.
But before you start any new physical activity, speak to your diabetes team. They can make sure you have all the information you need about how your diabetes might be affected. Especially if you treat your diabetes with insulin or certain diabetes medications like sulphonylureas, as being more active may increase your risk of hypos.
Your diabetes team will support you to make the right adjustments to your medications to reduce your risk of hypos.
Weight loss surgery
If you have a lot of weight to lose, ask your healthcare team if weight loss surgery is a possibility. There are different types of weight loss surgery, also called bariatric surgery. They aim to make you feel fuller sooner and eat less. Weight loss surgery can be a very effective way of losing weight, keeping your HbA1c in the target range and putting type 2 diabetes into remission for some people.
For people with diabetes, weight loss surgery isn’t just about weight loss. It is now seen as an actual treatment for type 2 diabetes, and the weight loss is a bonus.
Weight loss surgery changes the way the digestive system works, in ways that are helpful for people with type 2 diabetes. It can:
- change how the hormones in your gut work, which in turn affects how your body makes insulin
- increase the amount of bile acids that your body makes, these make your body more sensitive to insulin
- improve the way your body uses insulin, leading to lower blood sugar levels.
Diabetes weight loss medication
Your healthcare team may be able to prescribe some weight loss medications which can help with weight loss. One of these is Orlistat. Some diabetes medications, such as GLP-1 analogues, can also help with weight loss
Your healthcare team can give you advice about whether these medications are right for you. Avoid buying medications online and always get advice from a healthcare professional
Credit: diabetes.org.uk
Lilly releases Zepbound® (tirzepatide) single-dose vials, expanding supply and access for adults living with obesity
Team Metabolic Health
Eli Lilly and Company (NYSE: LLY) today announced Zepbound® (tirzepatide) 2.5 mg and 5 mg single-dose vials are available for self-pay for patients with an on-label prescription, significantly expanding the supply of Zepbound in response to high demand. The single-dose vials are priced at a 50% or greater discount compared to the list price of all other incretin (GLP-1) medicines for obesity. This new option helps millions of adults with obesity access the medicine they need, including those not eligible for the Zepbound savings card program, those without employer coverage, and those who need to self-pay outside of insurance.
“We are excited to share that the Zepbound single-dose vials are now here, further delivering on our promise to increase supply of Zepbound in the U.S.,” said Patrik Jonsson, executive vice president, and president of Lilly Cardiometabolic Health and Lilly USA. “These new vials not only help us meet the high demand for our obesity medicine, but also broaden access for patients seeking a safe and effective treatment option. In a clinical study, the 5 mg maintenance dose helped patients achieve an average of 15% weight loss after 72 weeks of treatment and has been a powerful tool for millions of people with obesity looking to lose weight and keep it off.”
Lilly has created a new self-pay pharmacy component of LillyDirect where patients with a valid, on-label prescription from the health care provider of their choice can purchase the vials. Distributing the vials via this channel ensures patients and providers can trust they are receiving genuine Lilly medicine, building on the company’s efforts to help protect the public from the dangers posed by the proliferation of counterfeit, fake, unsafe or untested knock-offs of Lilly’s medications. Lilly has also taken a vocal stance against the use of obesity medicine for cosmetic weight loss; a multi-step verification process will help ensure the vials are dispensed only to patients who have a valid, on-label electronic prescription from their health care provider. Patients can also purchase ancillary supplies, like syringes and needles, and will have access to important patient-friendly instructional materials on correctly administering the medicine via needle and syringe.
“People living with obesity have long been denied access to the essential treatment and care needed to manage this serious chronic disease,” said James Zervos, chief operating officer, Obesity Action Coalition. “Expanding coverage and affordability of treatments is vital to people living with obesity. We commend Lilly for their leadership in offering an innovative solution that brings us closer to making equitable care a reality. Now, it’s time for policymakers, employers and insurers to work with pharmaceutical companies to ensure no one is left behind in receiving the care they deserve and need.”
A four-week supply of the 2.5 mg Zepbound single-dose vial is $399 ($99.75 per vial), and a four-week supply of the 5 mg dose is $549 ($137.25 per vial) – less than half the list price of other incretin medicines for obesity and in line with the Zepbound savings program for non-covered individuals. The self-pay channel enables a transparent price by removing third-party supply chain entities and allowing patients to access savings directly outside of insurance.
“Despite obesity being recognized as a serious chronic illness with long-term consequences, it’s often misclassified as a lifestyle choice, resulting in many employers and the federal government excluding medications like Zepbound from insurance coverage,” said Jonsson. “Outdated policies and lack of coverage for obesity medications create an urgent need for more innovative solutions. Bringing Zepbound single-dose vials to patients will help more people living with obesity manage this chronic condition. We will also continue to advocate for a system that better aligns with the science.”
In a clinical study, tirzepatide 5 mg, along with a reduced calorie diet and increased physical activity, achieved an average of 15% weight loss over 72 weeks compared to 3.1% for placebo. Zepbound is the first and only obesity treatment of its kind that activates both GIP (glucose-dependent insulinotropic polypeptide) and GLP-1 (glucagon-like peptide-1) hormone receptors. Zepbound tackles an underlying cause of excess weight. It reduces appetite and how much you eat. Zepbound is indicated for adults with obesity, or those who are overweight and also have weight-related medical problems, to lose weight and keep it off. Zepbound should be used with a reduced-calorie diet and increased physical activity. It should not be used in children under 18 years of age or with other tirzepatide-containing products or any GLP-1 receptor agonist medicines. Zepbound has not been studied in patients with a history of pancreatitis, or with severe gastrointestinal disease, including severe gastroparesis, and it is unknown if patients with a history of pancreatitis are at higher risk for developing pancreatitis on Zepbound.
Zepbound is also available in 2.5 mg, 5 mg, 7.5 mg, 10 mg, 12.5 mg, or 15 mg per 0.5 ml doses in a single-dose pen (autoinjector). The recommended maintenance dosages are 5 mg, 10 mg, or 15 mg injected subcutaneously once weekly.
Credit: lilli.com
How carnitine transporters boost reproductive health
Team Metabolic Health
Understanding how carnitine transporters regulate sperm motility and hormone production could unlock new fertility treatments, offering hope for millions affected by infertility globally.
Carnitine transport mediated by multiple SLCs is depicted with different colors. The transport of carnitine across epithelial cells of the intestine, kidney, and placenta, as well as into the liver, brain, heart, muscle, epididymis, and airway tissues, is shown. OCTN2 (Green): mediates carnitine transport by a sodium-dependent mechanism, which is not reported for the sake of clarity. CT2 (Purple): involved in carnitine transport, specifically in the epididymis, contributing to sperm maturation. OCTN1 (Yellow): Low-affinity carnitine transporter participates in carnitine transport in various tissues. ATB0,+ (Blue): mediates sodium and chloride-dependent transport of carnitine, not reported for the sake of clarity, in the intestine and other tissues. MCT9 (Pink): transporter associated with carnitine efflux through the basolateral membrane of absorption epithelia like intestine and kidney. Arrows indicate the direction of carnitine transport across cellular membranes. Image created using Adobe Illustrator. Human transporters are represented as space-fill models from AlphaFold.
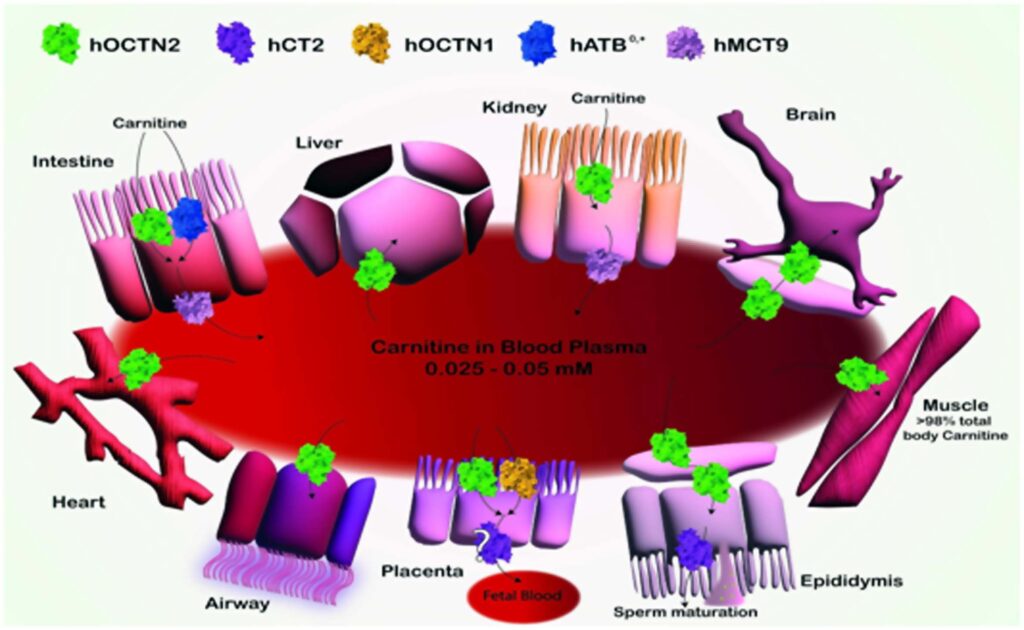
Schematic Representation of Carnitine Transport and Distribution in Various Tissues.
A recent study published in the journal Biochemical Pharmacology reviewed the role of membrane transporters in carnitine homeostasis, focusing on the molecular mechanisms involved and the implications in fertility. Carnitine is a crucial molecule in metabolism. It primarily drives fatty acid β-oxidation within mitochondria and plays a significant role in maintaining metabolic flexibility. Diet is the primary source of carnitine in humans, with only a small fraction being endogenously synthesized. The biosynthesis of carnitine requires the flux of its intermediates through different organelle membranes, and the majority of carnitine synthesis occurs in the liver, with additional synthesis in the kidneys and brain. As such, carnitine and its metabolites are distributed to tissues and organelles by membrane transporters.
Carnitine’s role in brain health: Besides fertility, carnitine is implicated in brain plasticity and cognitive functions, with acetylcarnitine influencing gene expression through histone acetylation.
The primary carnitine shuttle system in mitochondria comprises two enzymes (carnitine palmitoyl transferase 1 [CPT1] and CPT2) and an inner mitochondrial membrane transporter, carnitine/acylcarnitine carrier (CAC), also known as solute carrier 25 member 20 (SLC25A20). CAC is crucial for transporting acylcarnitines into mitochondria for β-oxidation. Notably, no redundant mitochondrial transporter compensates for CAC deficiency, making it indispensable for cellular life. Other carnitine shuttles are active in the endoplasmic reticulum and peroxisomes.
The coordination of peroxisomal and mitochondrial carnitine shuttles is essential for fatty acid catabolism. Carnitine has been implicated in modulating the acetyl-coenzyme A (CoA)-to-CoA ratio, which profoundly impacts lipid biosynthesis, gene expression, and carbohydrate metabolism. In the present study, researchers reviewed the role of transporters in carnitine traffic, focusing on the relationship between carnitine and fertility.
Carnitine network and alterations
Carnitine distribution is highly variable across tissues, ranging from low millimolar levels in most tissues to the highest (60 mM) in the testes. Many transporters are involved in maintaining carnitine homeostasis. Diet plays a crucial role in carnitine distribution; in fish and meat consumers, dietary carnitine accounts for about 75% of the total carnitine content. In contrast, vegans and vegetarians often rely heavily on endogenous synthesis and renal reabsorption for maintaining carnitine levels. Without supplements, vegans and vegetarians may experience reduced carnitine levels.
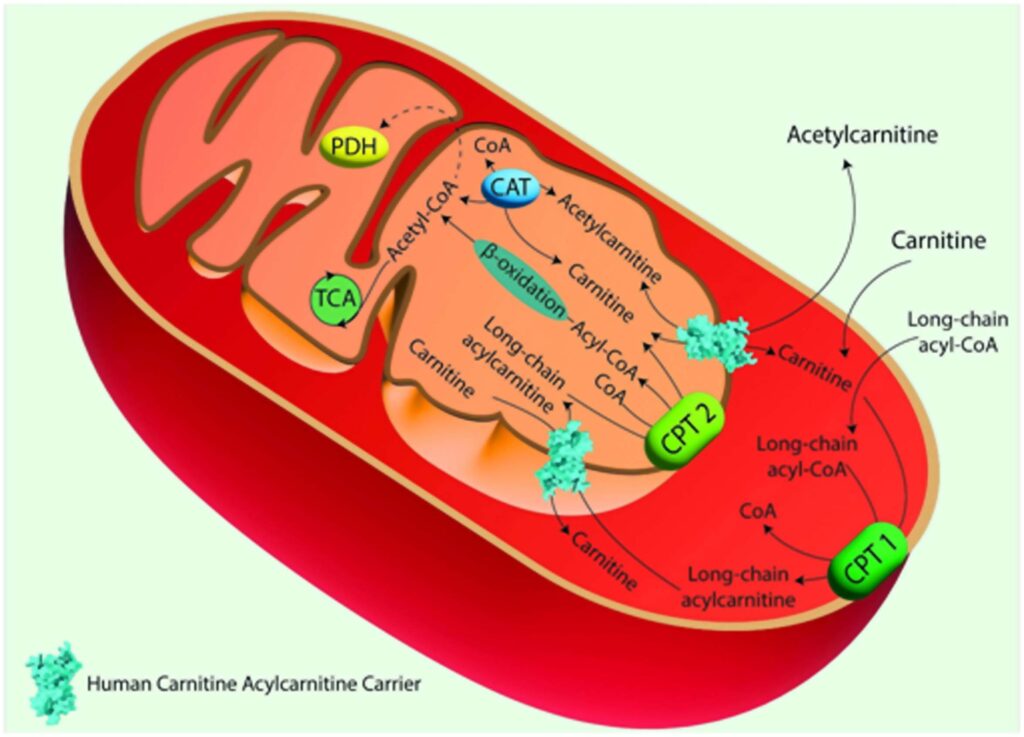
The Carnitine Shuttle in Mitochondrial Fatty Acid Oxidation.
Acyl-CoA synthase catalyzes the conversion of long-chain fatty acids into fatty acyl-CoAs. These are then converted to acylcarnitines by Carnitine Palmitoyl Transferase 1 (CPT 1), which is located in the outer mitochondrial membrane. Acylcarnitines are transported across the inner mitochondrial membrane by the Carnitine/Acylcarnitine Carrier (CAC) in exchange for free carnitine. Once inside the mitochondrial matrix, Carnitine Palmitoyl Transferase 2 (CPT 2), located on the inner mitochondrial membrane, converts acylcarnitines back into acyl-CoAs and free carnitine. The free carnitine is transported to the cytosol by the CAC, and it can be recycled by CPT 1. The acyl-CoAs imported into the mitochondrial matrix through the carnitine shuttle are subjected to β-oxidation, producing acetyl-CoA, which can then enter the TCA. Image created using Adobe Illustrator. hCAC is represented as space fill model from AlphaFold prediction
As such, endogenous synthesis and reabsorption may be more relevant for homeostasis. Renal reabsorption of carnitine is the primary means of compensating for dietary carnitine deficiencies. Organic cation/carnitine transporter 2 (OCTN2) facilitates carnitine reabsorption in the kidneys; mutations in OCTN2 lead to primary carnitine deficiency (PCD), a disorder characterized by systemic carnitine depletion and associated clinical manifestations, including muscle weakness, cardiomyopathy, and infertility. PCD treatment involves lifelong carnitine supplementation.
Carnitine deficiency in autism: Mutations in enzymes involved in carnitine biosynthesis have been linked to autism spectrum disorders, indicating a broader systemic impact of carnitine beyond fertility.
Secondary carnitine deficiencies (SCDs) may occur due to inherited defects in CPT2, CAC, or acyl-CoA dehydrogenases. Notably, CAC defects often result in life-threatening conditions due to impaired mitochondrial β-oxidation, leading to increased fatty acid accumulation in the cytoplasm. There are no redundant carnitine transporters to compensate for CAC defects. Therefore, early intervention is paramount for CAC deficiency. Treatment strategies for SCDs include diet-induced hypoglycemia prevention, carnitine supplementation, and medium-chain fatty acid diets.
Carnitine and Oxidative Stress in Infertility
Oxidative stress plays a pivotal role in both male and female infertility, with reactive oxygen species (ROS) and reactive nitrogen species (RNS) contributing to lipid peroxidation, DNA fragmentation, and reduced sperm viability. Carnitine, with its antioxidant properties, helps mitigate oxidative damage by scavenging free radicals, protecting sperm mitochondria from oxidative stress, which is particularly important in the preservation of sperm motility and overall fertility. The study also highlights how the antioxidant function of carnitine is crucial in managing oxidative stress in female reproductive tissues, such as the ovaries, where ROS imbalances can impair oocyte quality and disrupt the endometrial environment.
Human infertility
Globally, infertility is a significant concern, affecting over 180 million couples. Historically, it was predominately attributed to females; however, contemporary insights highlight a significant male contribution. The cause of infertility remains unexplained in many cases despite diagnostic advances. Mitochondrial dysfunctions are emerging as a common factor in both male and female infertility, linking energy metabolism to reproductive health. Lifestyle choices influence fertility, with evidence linking alcohol, obesity, and smoking to poor semen quality and ovulatory function.
Further, despite multiple studies on the relationship between male fertility and carnitine, the underlying molecular mechanisms remain elusive. In the male reproductive system, carnitine facilitates mitochondrial energy metabolism, particularly by regulating the acetylcarnitine/CoA ratio, which putatively is responsible for sperm concentration and motility. This regulation is particularly important in sperm maturation, where carnitine concentrations increase dramatically from the epididymal head (5 mM) to the tail (60 mM).
Some studies have suggested that lumen carnitine may stabilize the plasma membrane of sperms, enhance survival, and mitigate acrosome-reacted sperms, which are critical for successful fertilization.
The role of carnitine in females is less clear. However, carnitine is involved in the energy supply necessary for ovulation, folliculogenesis, and embryonic development. Mitochondrial dysfunction, exacerbated by carnitine deficiency, has been implicated in conditions like polycystic ovary syndrome (PCOS) and endometriosis. Therefore, carnitine deficiency could result in suboptimal energy, compromising oocyte quality and reducing the fertilization potential. Furthermore, carnitine has been shown to influence the production of sex hormones such as testosterone, estrogen, and progesterone, which are crucial for reproductive health.
SLCs in the carnitine network
Studies indicate that OCTN1 might function as a carnitine transporter in tissues with high carnitine levels, such as the epididymis. However, direct links between OCTN1 and infertility have not been studied so far. OCTN2 is the highest-affinity carnitine transporter. It is ubiquitously expressed in the heart, skeletal muscle, kidneys, and intestine. Mutations in OCTN2 are associated with Crohn’s disease (CD) due to carnitine deficiency in the intestinal epithelium. Further, mutations in OCTN2 can lead to fertility issues by disrupting carnitine homeostasis in the reproductive system, particularly in the epididymis. In the male reproductive system, carnitine transporter 2 (CT2) is localized in the luminal membrane of epididymal cells and the plasma membrane of Sertoli cells in the testes. In females, CT2 is highly expressed in the endometrium.
CT2 localization in the testes is the primary molecular link between male infertility and carnitine; however, its presence in the endometrium or testes does not clarify whether carnitine is associated with transporter regulation or energy requirements. CAC is an indispensable protein for cellular life. While the study points to CAC’s potential role in infertility, no direct causal mutations linking CAC to fertility dysfunction have been confirmed yet.
Clinical Implications
The study concludes by suggesting potential treatment avenues. Carnitine supplementation has shown promise in improving sperm motility and morphology in idiopathic infertility cases, while its role in antioxidant defense highlights its therapeutic potential in oxidative-stress-related reproductive disorders. Recognizing the role of carnitine and SLCs in sperm motility and energy metabolism could help develop advanced, more refined diagnostic tools and targeted therapies. Further research is necessary to understand the exact molecular mechanisms linking carnitine transporters and reproductive health, which could lead to novel treatments for both male and female infertility.
Credit: news-medical.net
GLP-1 drugs protect brain health by improving neurovascular function and reducing inflammation
Team Metabolic Health
New research reveals how GLP-1 receptor drugs, known for treating diabetes and obesity, also protect the brain’s vital neurovascular system, offering hope for tackling cognitive decline and neurodegenerative diseases like Alzheimer’s.
In a recent review published in the journal Cell Metabolism, a group of authors explored how Glucagon-Like Peptide-1 receptor (GLP-1R) agonism shapes the neurovascular unit (NVU), potentially linking metabolic health improvements to enhanced brain health.
Background
GLP-1R agonists protect the blood-brain barrier (BBB): These drugs help maintain the integrity of the BBB by preventing tight junction degradation, which can reduce the risk of neuroinflammation and cognitive decline.
Overconsumption of readily available, nutrient-rich foods has created an environment of overnutrition, leading to health issues like obesity and metabolic syndrome. Chronic low-grade inflammation, often associated with obesity, contributes to neurodegenerative diseases. GLP-1R agonists have emerged as effective tools for managing weight by influencing appetite and addressing metabolic dysfunctions. GLP-1R agonism not only helps with weight management but also appears to provide neuroprotective effects, including reducing neuroinflammation and enhancing brain health. Further research is needed to clarify whether GLP-1R agonism impacts brain health directly or through improved metabolic function.
The role of GLP-1 in metabolic regulation
GLP-1 is a hormone produced both in the gut and the brain. It plays a key role in maintaining glucose homeostasis by increasing insulin secretion and reducing glucagon levels post-meal. This incretin hormone also delays gastric emptying, thereby slowing glucose absorption and preventing sharp rises in insulin levels. Beyond its metabolic functions, GLP-1 is involved in regulating various behaviors, including feeding, fluid intake, and even motivated behaviors like drug consumption. Importantly, GLP-1 receptors are found not only in neurons but also in glial cells, which mediate its effects on brain health by regulating energy balance and maintaining neural circuits.
GLP-1R agonists in obesity management
GLP-1R agonists, such as semaglutide, liraglutide, and tirzepatide, have gained prominence in the treatment of obesity. These drugs work by mimicking the action of endogenous GLP-1 but at supraphysiological doses, resulting in stronger and longer-lasting effects on appetite suppression. While endogenous GLP-1 has a short half-life and limited ability to act on distant organs, exogenous GLP-1R agonists have proven highly effective in reducing food intake and promoting weight loss.
Obesity is a significant risk factor for a range of chronic conditions, including type 2 diabetes and cardiovascular diseases. Individuals with obesity often experience chronic low-grade inflammation, which not only affects peripheral tissues but also has detrimental effects on brain health, linking obesity to neurodegenerative diseases.
Chronic inflammation, obesity, and brain health
Chronic inflammation, a hallmark of obesity, is associated with an increased risk of developing neurological conditions, including cognitive decline and neurodegeneration. The inflammatory state extends to the brain, contributing to conditions such as Alzheimer’s disease (a neurodegenerative disorder characterized by progressive memory loss and cognitive decline). This inflammatory process involves activation of microglia and astrocytes—glial cells critical for immune responses in the brain. The neuroinflammatory processes observed in obesity are similar to those seen in neurodegenerative diseases, with microglial activation, reactive astrogliosis, and insulin resistance playing key roles.
Neuroprotective effects of GLP-1R agonism
GLP-1R agonists improve cerebral blood flow (CBF): By enhancing neurovascular coupling, these drugs ensure that blood flow is properly regulated in response to brain activity, improving overall brain function, particularly in obesity and metabolic disorders.
Beyond their role in weight management, GLP-1R agonists have shown neuroprotective and neurotrophic properties, offering potential benefits in reducing neuroinflammation. GLP-1R signaling in microglia helps reverse the polarization of these immune cells from a pro-inflammatory state to an anti-inflammatory state, thus reducing neuroinflammation. GLP-1R agonism has been observed to reduce microglial activation, a key driver of neuroinflammation, and to protect against neuronal damage. Furthermore, these agonists may improve brain insulin sensitivity, reduce oxidative stress, and promote the survival of neurons.
Recent studies suggest that GLP-1R agonists may influence the neurovascular unit (NVU), the critical interface where neurons, glial cells, and blood vessels interact to maintain brain function. The NVU plays a pivotal role in ensuring proper blood flow to the brain, regulating nutrient supply, and removing waste products. Dysfunction in the NVU is linked to both metabolic disorders and cognitive decline.
GLP-1 and the NVU
GLP-1 receptors are expressed on various cell types within the NVU, including neurons, astrocytes, microglia, and endothelial cells. Activation of these receptors by GLP-1R agonists has been shown to confer protection against microvascular damage, particularly in models of diabetic retinopathy and stroke. Given the similarities between the brain’s and retina’s vascular systems, these findings suggest that GLP-1R agonism could also protect the brain’s microvasculature, preserving the integrity of the blood-brain barrier and improving cerebral blood flow.
In models of high-fat diet-induced obesity, GLP-1R agonism has demonstrated the ability to enhance neurovascular coupling, improving the relationship between neuronal activity and blood flow in the brain. This may counteract the neurovascular dysfunction caused by chronic overnutrition. These findings suggest that GLP-1R agonists may help counteract the adverse effects of overnutrition on brain health.
Implications for neurodegenerative diseases
The potential for GLP-1R agonism to protect the brain and improve cognitive function has spurred interest in its use as a therapeutic strategy for neurodegenerative diseases like Alzheimer’s. Preclinical studies have demonstrated that GLP-1R agonists can reduce the accumulation of amyloid plaques, a hallmark of Alzheimer’s disease, and improve synaptic function. In addition, GLP-1R agonists have been observed to enhance the health of endothelial cells in the brain, promoting vascular remodeling, which may further support cognitive function.
Additionally, the ability of GLP-1R agonists to modulate the NVU and reduce neuroinflammation suggests that they could slow the progression of neurodegenerative diseases. By improving the health of the brain’s vasculature and reducing inflammatory responses, GLP-1R agonists may help preserve cognitive function in individuals with metabolic disorders or neurodegenerative conditions.
Conclusions
To summarize, the connection between metabolic and cognitive health highlights brain-body communication, redefining some disorders as neurometabolic. Repurposing antidiabetic drugs like GLP-1 mimetics for neurological diseases is gaining interest, as metabolic disorders pose a significant risk for neurodegeneration. GLP-1 mimetics show promise due to their anti-inflammatory, neuroprotective, and neurotrophic properties. The expression of GLP-1R on various cell types and its impact on the neurovascular unit (NVU), including neurons, glial cells, and endothelial cells, make GLP-1 a strong candidate for bridging brain-body crosstalk.
Credit: news-medical.net
Living with obesity – and what it means for your heart and general health
Team Metabolic Health
Obesity is a risk factor for a number of complications. Some of these are cardiovascular, a group that includes coronary artery disease, high blood pressure, stroke, hyperlipidaemia, heart attack and heart failure.1 Obesity is also a leading cause of cardiovascular mortality and morbidity.1 Here is the good news: With appropriate action, supported by professional guidance and advice, the cardiovascular risk factors may be managed and reduce chance of complications.
Clarifying a few important terms
This blog post is about how obesity affects health, with a particular emphasis on so-called cardiovascular complications of obesity. The last part of that might sound a bit cryptic, so let’s begin by clarifying a few important terms. It’s actually quite simple.
“Cardio” means related to the heart, while “vascular” means related to the blood vessels.
Thus, cardiovascular complications, for instance, is simply a way to refer to a cluster of issues that primarily affect the heart and blood vessels.
Living with obesity tends to increase the risk of developing cardiovascular complications or even suffering a cardiovascular event such as stroke or heart attack.1
But consider this: Obesity doesn’t define anyone. It’s a condition and a disease for which there are genetic as well as biological, behavioural, psychosocial and environmental reasons2 – true! But that doesn’t make obesity irreversible or inescapable.
A closer look at cardiovascular complications
Obesity is a disease that increases the risk of unintended cardiovascular health consequences3. It happens to be a rather critical one. In fact, obesity is among the leading causes of elevated cardiovascular disease, mortality and morbidity1. This video might help you to understand it better:
Obesity may do more than that
Unfortunately, that’s true. In fact, obesity may increase the risk of developing over 200 complications5, including type 2 diabetes, asthma, cancer, liver and gallbladder disease, sleep apnea, osteoarthritis and gynaecological complications1.
But let’s focus on those affecting the heart and blood vessels such as ischaemic heart disease, coronary artery disease and hypertension1 – the latter being a cardiovascular risk factor in its own right, potentially leading to stroke, heart attack and heart failure.1
Admittedly, the relationship between obesity and its potential cardiovascular consequences is a serious one. But every cloud has a silver lining.
Let’s switch gears and focus instead on the…
Reasons to be hopeful
While the consequences of living with obesity could be serious, steps towards reducing your risk can be taken. Doctors trained in obesity care know what kind of action yields positive results. We are collectively much smarter about obesity today than we once were.
Many people living with obesity can, for instance, learn from a properly trained obesity care provider. But the opposite is also true. Many doctors can learn from those affected by obesity – about how different treatment strategies are experienced at the individual level, for instance, mentally and physically. You can read more about it here.
A significant step in the direction of a healthier future
The fact that the medical and scientific community have conclusively shown that obesity is a disease is really cause for celebration! Why? Because it means we are significantly closer to being able to address it optimally.
For anyone affected by obesity, reaching out to carefully trained obesity care providers for advice and guidance can make a difference. Such specialists can help outline a personalised weight management strategy – one that takes stock of obesity’s multifactorial nature and doesn’t ask more of you than is appropriate and reasonable.
Why weight loss is helpful
Doctors have found that weight loss can benefit the heart. For example, losing 5% of one’s body weight has been associated with significant and long-standing health benefits7-18. These include reduced blood pressure19, leading to improved heart health.
And while some complications are more sensitive to weight loss than others, increasing weight loss beyond 5% may lead to additional improvements in obesity-related complications7-18. In a study involving people with type 2 diabetes, weight loss of 5–10%, for instance, was shown to produce improvements in cardiovascular risk factors a year after the weight loss.
Continue – or begin – your weight management journey today!
Remember, change starts with you. But it doesn’t have to end with you – not if you do the smart thing and reach out to those who have a professional, scientific understanding of genes, metabolism, human psychology and all the other complexly interwoven factors of obesity.
By doing that, healthy change can continue to benefit you – in the form of sustained weight loss and reduced cardiovascular risk factors now and in the future.
We wish you success with your next steps to better health.
Credit: truthaboutweight.global
Bitter pill: 20% of doctors obese, 53% diabetic, 24% hypertensive
Team Metabolic Health
SURVEY POINTS TO HIGH PREVALENCE OF LIFESTYLE DISEASES AMONG DOCS
Ahmedabad : They are advocates of balanced diet, exercise and healthy lifestyle, but a study conducted in the state reveals high prevalence of lifestyle diseases among doctors.
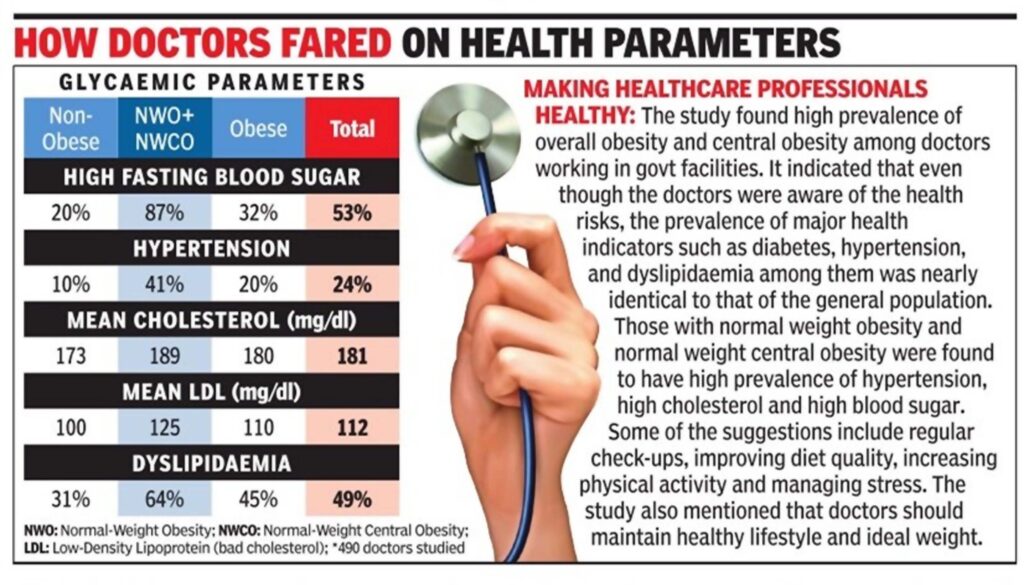
The MP Shah Medical College in Jamnagar surveyed 490 doctors working in govt facilities and found that 20% of them were obese, 53% were diabetic and 24% were hypertensive. According to several medical organisations, while there is no comprehensive study on private practitioners, the results could be the same for them as well, with a high prevalence of lifestyle diseases.
The study titled Prevalence of Normal Weight Obesity and Its Cardiometabolic Implications Among Government Doctors in Gujarat, India: A Cross-Sectional Study, by Yogesh M, Nidhi Trivedi, Naresh Makwana, P Hari Priya, PVM Krishna, and Kadalasaru D, from the Department of Community Medicine at the MP Shah Medical College, Jamnagar, was published recently in the journal Clinical Diabetes and Endocrinology.
Researchers measured various parameters for doctors in the govt medical setup, including Body Mass Index (BMI), blood pressure, fasting glucose and lipids. The results showed that only 10% of doctors fell into the normal weight category. While 20% were found to be obese, 26.5% of those surveyed had normal weight obesity (NWO) where the BMI is 18.5–24.9 kg/ m2 with high body fat per cent, and 21% had normal weight central obesity (NWCO) where the BMI is 18.5–24.9 kg/ m2 with high waist circumference. The rest had both NWO and NWCO, the study said.
“Regarding the lipid profile, the mean total cholesterol (TC) and low-density lipoprotein cholesterol (LDLC) levels were highest in the NWO+NWCO groups,” the study mentioned. It said that the prevalence of obesity mirrors the trend observed in National Family Health Sur veys —from 11.8% in 1998, it had increased to 31.3% in 2016.
“Doctors are increasingly falling victim to lifestyle diseases. A major factor is stress, especially in the 30-50 years age group,” he said. “Doctors face the same risk factors as the general population when it comes to lifestyle-related diseases, with their eating habits and long working hours,” said Dr Dhiren Shah, president of the Ahmedabad Medical Association (AMA).
Credit: The Times of India
Is Nighttime Depression Really a Thing?
Team Metabolic Health
There are lots of reasons your mood might tank at night. Here’s how to address the bedtime blues.
It’s not uncommon for our minds to unleash a torrent of difficult feelings under the cover of darkness: sadness and negative thoughts may surface at night, making sleep hard to come by.
On social media and elsewhere people often refer to this as “nighttime depression.” But is that really a thing? And if so, why do some people get blue at night?
Feeling down after dusk doesn’t necessarily mean that you have a mental health condition, experts said. Understanding why it happens can help you take steps to feel better.

Credit: Getty Images
What is nighttime depression?
Nighttime depression is a colloquial term for depressive symptoms that either appear or worsen late at night. It is not itself a diagnosis.
While anxiety can also ramp up at night, and tends to make people feel agitated, tense and restless, nighttime depression is best characterized as a low mood.
“It’s a sense of sadness,” said Dr. Theresa Miskimen Rivera, a clinical professor of psychiatry at Rutgers University and president-elect of the American Psychiatric Association. “It’s that feeling of: There’s no joy. My life is so blah.”
Nighttime depression can also feel uncomfortable — “not only in your mind, but in your body,” Dr. Rivera added, especially if these feelings interfere with getting enough sleep.
Why would nighttime affect your mood?
There are many factors that can tank your mood late at night, including insomnia, loneliness, alcohol or drugs. But our circadian rhythms, or body clock, also play a role.
Our body clock is what helps control when we feel alert in the morning, hungry at mealtimes and sleepy at night. It also helps regulate important processes like body temperature, hormone levels and the immune system. Circadian rhythms control the beginning of your “biological night,” telling your pineal gland to make melatonin, a hormone that helps induce sleep.
And if your body clock isn’t aligned with your sleep-wake cycle, it can have negative effects on mood.
Studies of night workers, for example, have found that working outside of regular business hours is associated with an increased risk of depression and anxiety, among other health problems.
Although nighttime depression can be a symptom of clinical depression, research suggests that most people, including those without mood disorders, will feel worse as a result of staying up too late or waking up too early.
One study of 21 healthy adults measured positive and negative emotions at four-hour intervals and found that negative feelings peaked in the middle of the night at around 3 a.m.
Another small study used a different type of measurement called a visual mood scale to assess how participants felt every hour and showed a connection between circadian rhythms and symptoms of a depressive-like mood. In the study, low mood rose throughout the night and peaked around 8 a.m.
These feelings may peak earlier for people who are naturally early risers.
What can you do to feel better at night?
To head off symptoms of depression at night, start with the basics of good sleep hygiene.
Dr. Sarah L. Chellappa, an associate professor at the University of Southampton who has studied the relationship between circadian rhythms and mood, recommended establishing consistent sleep and wake times, avoiding daytime naps and stashing electronic devices at least an hour before bedtime. Keeping your bedroom at a comfortable, cool temperature is also important.
If you are feeling low at night despite taking those steps, think about what might have led to your discomfort.
Is there a physical reason?
Did you, for example, have too much coffee today, drink alcohol or eat a heavy meal right before bed? These things can get in the way of a good night’s rest, which can in turn lead to depressive symptoms.
Is there something weighing on your mind?
Dr. Rivera advised keeping a pen and paper by your bedside to jot down any thoughts and then taking a fresh look during the day. This allows you to address your concerns later, because there is usually very little to be done about them at 2 a.m.
Try to avoid making any judgments or decisions when you’re awake at night and instead focus on less serious things, advised Dr. Alfred J. Lewy, a professor emeritus of psychiatry at Oregon Health & Science University and an expert on melatonin and circadian rhythms.
“When you wake up in the morning, your mood should brighten, and you should have a less pessimistic outlook on what you were so distraught about a few hours earlier,” he said.
If you find that your low mood isn’t improving during the day and instead persists continually for weeks, then it’s important to seek help from a health care provider, the experts said.
And if your feelings at night become severe and include fear, paranoia, irritability, impulsivity or suicidal thoughts then it’s necessary to seek care quickly or call 988, the national suicide hotline, Dr. Rivera said.
Credit: The New York Times
Obesity real risk for blood sugar: Why weight loss drugs are preventing other diseases too
Team Metabolic Health
Here are key takeaways from latest research and a session of the European Association of the Study of Diabetes (EASD)
If there is one takeaway from latest research and the European Association of the Study of Diabetes (EASD) session in Madrid, which I attended, it is that researchers are unanimous about the benefits of weight loss. Obesity is at the centre of our disease burden and the blockbuster weight loss drugs have indeed shown multiple protective benefits that help users drop body fat between 10 and 20 per cent.
A GLP1 receptor agonist, semaglutide mimics the incretin hormone in the gut to stimulate insulin production in response to sugar overload. (File)
CAN WEIGHT LOSS DRUG SHIELD YOU FROM COVID EFFECTS?
The most significant finding was that people without diabetes, who took injectable semaglutide (brand name Wegovy) for weight loss, were less likely to die of COVID-19. The study, published in the journal of the American College of Cardiology, showed users could lower their mortality risk by as much as 33 per cent.
A GLP1 receptor agonist, semaglutide mimics the incretin hormone in the gut to stimulate insulin production in response to sugar overload. We know that fat cells have a lot of receptors for the Covid virus, so obesity is definitely high risk. Apart from weight reduction, it boosts functioning of the kidney, liver, and perhaps the immune system, all of which can reduce severity of a virus infection.
BETTER OBESITY CONTROL
The once-weekly shot of tirzepatide (brand name Mounjaro), which combines GLP-1 and GIP mimicking hormones, to regulate blood glucose levels and even ensure fat burn. Across all doses and trials, women users lost up to 24.6 per cent of their body weight compared to 18.1 per cent in men. This is a huge drop. The findings, presented at EASD, could lead to more personalised and lasting treatment plans.
WHAT CHANGED WITH WEIGHT LOSS DRUGS?
Other studies have shown that Wegovy can reduce heart-disease-related death by 20 per cent. Although some questions were raised about confounding factors — whether those who were treated with these drugs had a better profile before they used them — most agreed that such drugs were pluripotent. Which means that these are equally effective in preventing other conditions like cancer and brain disorders. They are now being studied for inducing changes in eating behaviour, like snacking, which has been shown to come down drastically among users. Studies are ongoing to assess if there is reduction in liver fat and improved kidney functioning post the drug-induced weight loss.
DIABETES REMISSION POSSIBLE IF YOU MANAGE PREDIABETES
My paper was on reversing prediabetes — a condition when your sugar levels are elevated but not high enough to qualify as diabetes. At the stage of prediabetes, the pancreatic beta cell function (which regulates insulin secretion) is much better preserved. So the insulin resistance is not as high as in the stage of diabetes.
We have shown that South Asians, including Indians, in the stage of prediabetes needed to reduce their weight by just 2.5 kg to achieve reversal and subsequent diabetes remission. A remission of five years at this early stage means benefits could extend to 10 to 15 years.
This kind of weight loss can be achieved by stepping up on normal aerobic exercises. Our studies have shown that even a 10 per cent reduction in carbohydrate intake can help achieve remission with a compensatory 10 per cent increase in the protein intake. If the calorie restriction is continued for a longer period, say two to three months, then the fat in the pancreas begins to melt. As a consequence, the pancreatic insulin secretion by the beta cells improves. Over time a person can achieve remission.
Credit: The Indian Express
Novo’s GLP-1 Wegovy could improve heart health for millions more than previously thought, AI study finds
Team Metabolic Health
Through real-world data, an AI company found that popular weight loss drugs could be a preventive measure for patients at risk of heart attack and stroke.
Novo Nordisk got a major boost in March when the FDA approved its GLP-1 diabetes and weight loss drug Wegovy to also prevent heart attacks and strokes in patients with certain risk factors. The decision opened the market up to more than six million people and broadened Medicare coverage for the blockbuster drug, now on track to become one of the best-sellers of 2024.
And that may only be the tip of the iceberg, according to a sweeping AI study from Dandelion Health, which identified an additional 44 million lower-risk cardiovascular patients who could benefit from a GLP-1 treatment, hinting at the potential to greatly expand insurance coverage.
Scott Olson via Getty Images
Putting AI to work
Dandelion leaders ran the study as a proof-of-concept test of their real-world data platform, which uses commercial and academic AI programs to analyze patient information obtained through revenue-sharing agreements with health systems, including Sanford Health, Sharp HealthCare and Texas Health Resources. The platform could be a faster and less expensive way to deliver results than traditional clinical trials. Studies could take weeks, not years, and incorporate larger and more diverse patient groups, according to the company’s co-founder and CEO, Elliott Green.
“No one ever does preventative trials because they’re just too big,” he said. “But this AI proof-of-concept started to show that there’s a path forward to being able to achieve that.”
Mining real-world data
For the observational study, Dandelion examined whether GLP-1 use might reduce the risk of major adverse cardiac events such as heart attack or stroke in overweight and obese patients. The study used inclusion criteria similar to the Novo Nordisk-sponsored trial that helped convince the FDA that Wegovy had heart benefits. But, unlike SELECT, Dandelion’s patient group didn’t have severe preexisting cardiovascular disease.
Researchers applied an AI algorithm from Pheiron trained to spot cardiovascular risk indicators on patient electrocardiograms. The AI assigned patients a risk score and compared predicted risk for heart attacks and strokes in GLP-1 users versus non-users. The results expanded on the findings of Novo’s trial, which found Wegovy reduced the risk of major cardiac events in the study group as much as 20%.
Bottom of Form
Dandelion’s study, seven times the size of Novo’s, determined that people in the lower-risk group who took GLP-1 drugs had 15% to 20% lower risk scores for major adverse cardiovascular events after taking the drug for three years. Treating these additional patients could head off 17,300 heart attacks and 16,700 strokes a year, according to study authors.
“With further validation, this AI-driven approach could potentially unlock a new biomarker or surrogate endpoint that measures [major adverse cardiovascular event] risk, enabling shorter and smaller clinical trials by predicting cardiovascular outcomes earlier without waiting for [adverse events] to occur,” they stated.
Speeding research
Real-world data-based AI could validate GLP-1s for broader applications, from neurological and liver diseases to addiction and arthritis.
Green said Dandelion already has another GLP-1 study in the works, using AI to assess muscle changes on patient abdominal CT scans to determine whether GLP-1 drugs also cause muscle to wither during weight loss. The platform could also help pharma companies explore and validate label expansion opportunities and perform other types of research. Dandelion is working with several companies, Green said.
“Clinical trials are very focused. You come in with a very specific question, and you get a very specific patient population,” Green said, noting that a broader approach is often too challenging due to time and cost constraints.
With AI, instead of looking at a limited area, similar to what you might see under a single street light, Green said, you can illuminate the whole neighborhood.
Credit: pharmavoice.com
As AI transforms drug development, biotechs might not need as much Big Pharma support
Team Metabolic Health
Small biotechs are making gains with AI drug development, and their advantages may help some push ahead without Big Pharma.
AI is making its mark on the pharma market, presenting opportunities for Big Pharma to cut down on drug development costs and fast-track new discoveries. But AI’s capabilities also open the door for smaller biotechs to remain independent rather than leaning on deep-pocketed, established pharmas, according to a report from S&P Global Ratings.
Big Pharma has been investing in AI and partnering with tech companies in recent years, and the area’s value could jump from $1 billion in 2022 to a projected $22 billion in 2027, according to data from Boston Consulting Group.
Getty Images
Many of the early investments in the space were focused on leveraging machine learning. For example, Pfizer teamed up with IBM Watson in 2016 to leverage the company’s machine learning system in drug discovery, while Merck & Co. and AstraZeneca partnered with Amazon Web Services in 2017 to develop a cloud-based drug discovery platform.
But the collaborations between pharmas, tech companies and biotechs have now “given rise to a new breed of AI-driven [biotech] entities,” according to the report.
This new breed has AI at the center of their platforms, but are still partnering with established pharmas to overcome high development costs. Independent AI biotechs will likely seek more partnerships and collaborations as a result, the report predicted, but also have the potential to break out on their own with treatments that could alter the commercial landscape.
“The relationship between AI biotechs and big pharma won’t necessarily be symbiotic,” the report stated. “The formers’ significant potential for innovation means they could yet emerge as competitors to pharmaceutical incumbents (and Big Pharma’s R&D functions).”
Already, several biotechs have drug assets in the clinic that were discovered through AI — both with and without Big Pharma contributions.
Lantern Pharma has several drugs in clinical trials that were discovered through its AI platform. Insilico Medicine has 31 programs and out-licensing agreements for a handful of candidates generated by AI.
AI’s big impact
While S&P didn’t expect that AI will cause an influx of blockbuster drugs, the ratings company forecasted AI biotechs to have a “considerable” impact on shortening the drug development process.
Bottom of Form
Instead of spending four to seven years in the discovery and preclinical stage, AI could shorten the timeline to two to three years, according to the report. Clinical development could be only three to five years long, shaved down from the current range of seven to nine.
The benefits of speed could help independent biotechs overcome the huge cost challenge of developing new drugs. Between 2022 and 2023, the cost of moving a new drug from discovery to launch averaged $2.3 billion, according to a report from Deloitte.
With an 85% compound annual growth rate projected for the global pharma-AI market, the technology will continue to expand its role across the industry. Still, investments in the space will take time to be fully realized. Instead, the gains are likely to be “incremental,” with efficiencies being slight, the report predicted.
“Drug discovery, with or without AI, will remain a complex and time-consuming practice characterized by experimentation, false starts and failures,” the report stated.
If AI platforms are able to help pharma companies pursue treatments for more complex diseases, working in those complicated arenas could also bog down drug development timelines and increase resource demand, S&P noted.
Credit: pharmavoice.com
AI Simulations Help Drug Trials
Team Metabolic Health
Artificial intelligence (AI) has been revolutionizing much of early drug discovery, yet human clinical trials remain a bottleneck. Now some applications of the new technologies are bringing efficiencies to clinical research.
Sophisticated modeling and simulations suggests that AI can play a major role in improving the success rates of novel drugs entering human studies. The pharmaceutical industry has long struggled with efficiency rates. According to the Congressional Budget Office (CBO), only 14% of drugs that enter clinical trials are ultimately approved by the FDA. The development process is complex and can take many years, with many drugs failing at various stages. Estimates are that the cost of developing one drug can be over $2 Billion.

AI helps clinical trials. Credit: GETTY IMAGES
The goal of modeling software in clinical research is to create programs that can simulate expensive clinical trials. Other technical industries use extensive simulations when building highly complex items like semiconductors and fighter jets. But in some ways, biology is actually harder to model due to the higher systemic complexity.
Simulations hold a multitude of promises for drug development. By pre-emptively modeling trials and getting accurate dosing, the probability of success can be improved and predictability increased. Ultimately, the moonshot is using trial simulations to be able to conduct completely safe patientless trials. Although completely virtual trials are still probably more than a decade away, machine learning and AI have advanced sufficiently to begin to manage human biology and data better.
QuantHealth, an AI-focused clinical trial design company based out of Tel Aviv, has announced the completion of more than 100 simulated clinical trials, reporting an 85% accuracy rate. The company has developed a proprietary AI-based Clinical-Simulator system that combines over 1 trillion data points across the clinical and pharmacological domains to optimize clinical development, according to CEO Orr Inbar.
The clinical trial simulation software enables scientists to holistically model a clinical trial with thousands of variations rapidly, allowing drug development experts to evaluate parameters on the basis of endpoint success, commercial viability, and protocol feasibility. The In-Silico platform generates evidence for how therapy will perform across all clinical phases, as soon as its mechanism is known, and preclinical evidence has been established. This synthetic evidence generation engine can be used to support trial planning, as well as indication selection, drug repurposing, and in-licensing asset evaluation.
In order to address the challenge of finding large swaths of data on which to train its models, AI companies have been working with health systems to gather data to train the model and QuantHealth has spent several years acquiring, processing and analyzing data from proprietary sources. QuantHealth has partnered with OMNY which represents data from 50 provider organizations nationally including hospital systems, nonprofits, community practices, pediatric hospitals and national cancer institutes that represent 78 million patients, or a third of Americans. They have licensed over 350 million patients’ data from databases to get a complete picture of each patient and added five more databases in genetics, cell biology, pharmacology, and biological cascades. The company builds a foundation using clinical trial results and FDA data, with elements of real world data (RWD), and clinical knowledge graphs and then incorporates sponsor’s own additional data.
QuantHealth’s AI can predict phase 2 trial outcomes with 88% accuracy (compared to the actual success rate of 28.9%), and phase 3 trial outcomes with 83.2% accuracy (versus the industry average of 57.8%) according to the company’s press releases and interviews. The technology is able to predict clinical trial outcomes with significantly higher accuracy than current success rates. The accuracy would allow users to answer mission-critical questions such as trial go/no-go, cohort optimization, drug repurposing, and more.
QuantHealth performs trial design for pharma companies and fine-tunes results by changing endpoints or population to determine different outcomes. It can be used for portfolio optimization, how well new drugs will perform against competitors when considering acquisitions, and health systems asking what patients will respond to different trials and their outcomes.
CEO Inbar states that QuantHealth works with five of the top ten big pharma companies, with most clients moving from pilots to multiple trials.

AI in drug research. Credit: GETTY Images
Another important area AI enhanced drug development simulations is accurately predicting appropriate dosing. Drugs are first tested in animals to confirm safety. But understanding how to move from animal doses to humans continues to be a difficult.
Certara is using AI to accelerate the drug development process by technology that can seamlessly incorporate simulations with other approaches to help model dosing based on prior non-human studies.
The US Food and Drug Administration (FDA) has had a long standing collaboration with a number of Certara software licenses for reviewing new drug and biologics applications. Additionally the FDA has awarded grants to expand its predictive models for assessing drug virtual bioequivalence (VBE) and to create a formulation toolbox for topically applied drugs. These capabilities will help enable safer, faster and more cost-effective product development of both complex generics and novel drugs.
AI helps Certara to mine millions of documents and unstructured data sources in a systematic and meaningful manner and also couple data that is in the public domain with a pharmaceutical company’s proprietary data to build a unique database. The AI platform mines about six million public sources, including massive regulatory databases and associated filings, memos, and scientific meetings.
Writing in Pharma Focus Europe, Amin Rostami-Hodjegan and Piet van der Graaf describe applications utilized at Certara. AI helps to manage information overload, particularly when the facts are sparse and seemingly unconnected, by going through data and extracting elements that are useful. It also gives Certara confidence in models by gathering indirect evidence that verifies the model-informed decisions. Certara uses AI to build models that are a mathematical representation of drug physiology and build a biological map. The models help address questions such as, “How long will the molecule stay in the body? Will it turn into an undesirable metabolite?”
Simulations are also used to predict clinical endpoints in discovery for novel mechanisms and to identify new biomarkers. The models can capture fundamental biology and then simulate what happens to the biomarkers, cell types, and cytokines when they put a compound into that system. This allows researchers to predict clinical endpoints for novel mechanisms earlier in the development process.
AI is providing growing support for the drug development process. Its applications range from reviewing millions of data points and gleaning relevant information, to helping build biological maps and models of new mechanisms of action and predicting clinical endpoints.
AI-based clinical simulation systems can be a game-changer for the pharmaceutical industry. The ability to predict clinical trial outcomes with significantly higher accuracy than current success rates, it has the potential to save the industry billions of dollars and years of time.
Credit: Forbes
Novo and Lilly contender Zealand Pharma heralds its obesity drug alternative: It’s our ‘crown jewel’
Team Metabolic Health
Key Points
- Danish biotech Zealand Pharma is targeting the “next generation” of weight loss drugs as competitors pile into a market dominated by heavyweights Novo Nordisk and Eli Lilly.
- CEO Adam Steensberg heralded early-stage trial results of its GLP-1 treatment in an interview with CNBC, but said it was the company’s separate obesity drug candidate that sets it apart.
- Zealand Pharma is now scouting for a pharma partner to help it target global markets, Steensberg said, even as takeover speculation mounts.

Jaap Arriens | NurPhoto
Danish biotech Zealand Pharma is targeting the “next generation” of weight loss drugs as competitors pile into a market dominated by heavyweights Novo Nordisk and Eli Lilly.
CEO Adam Steensberg told CNBC Thursday that early-stage trials of its experimental obesity injection point to higher-quality weight loss — with reduced muscle loss and fewer side effects — versus traditional GLP-1 treatments. The company is now scouting for a global pharma firm to partner with, he added.
“Our focus is really what’s needed in the 2030s, and it’s really about establishing, you can say, the next-generation molecules that are not based on GLP-1s,” Steensberg said.
Last month, Zealand Pharma announced positive top-line results from a phase 1b trial of its weight loss drug, a GLP-1/GLP-2 receptor dual agonist called Dapiglutide. It puts the company head-to-head with major obesity players Novo Nordisk and Eli Lilly, whose GLP-1s Wegovy and Zepbound, respectively, have exploded in popularity for their weight loss effects.
However, Steensberg said it’s the company’s separate obesity drug candidate, Petrelintide, a long-acting amylin analog, which could set it apart from the competition, offering an alternative for users who cannot tolerate GLP-1s.
“That’s what we call our crown jewel. This is the one where we have the highest expectations,” Steensberg said.
“We have a very strong feeling that this could become a foundational therapy in the future – something that provides the weight loss that patients are looking for but with the potential for a better tolerability profile,” he added.
Amylin analogs are a nascent form of weight loss treatment. They work by mimicking a hormone that is co-secreted with insulin in the pancreas to increase satiety. This differs from GLP-1 agonists, which mimic incretin hormones produced in the gut to suppress appetite and regulate blood sugar.
“It’s two very different human experiences,” Steensberg said, comparing GLP-1s with amylin analogs. “If you work on satiety, it will be a more pleasant experience. So once you get into it, you can stay long-term [on the] treatment.”
Novo Nordisk is also experimenting with its own version of the treatment, combining the GLP-1 component Semaglutide with amylin analog Cagrilintide in a candidate called CagriSema.
In June, Zealand Pharma also announced positive results from a phase 1b trial of Petrelintide, which showed that a course of 16 weekly injections reduced body weight by up to 8.6% on average.
The company said at the time that the findings showed “robust support” for the drug’s potential as an alternative to GLP-1s. Following the biotech firm’s first-half results in August, Steensberg upped the ante, saying amylin analogs have the potential to become “the future backbone therapy for weight management.”
“If we can develop a molecule that is giving patients the weight loss they’re looking for with a very benign tolerability profile, and we can also show risk reduction when it comes to cardiovascular health, I think we have all the reasons to believe it could become a first-line therapy,” Steensberg told CNBC in the interview Thursday.
Seeking a global pharma partner
Zealand Pharma, which was founded almost three decades ago with a focus on peptide-based medicines, has ridden a rising tide over recent months as it has ventured further into obesity treatments. So far this year, its share price is up more than 110%.
Competition in the sector is fierce, however, with Novo Nordisk and Eli Lilly still dominating the market as their so-called miracle drugs become essential to consumers across the globe.
Several drug regulators, including in the U.S. and European Union, have now expanded GLP-1 drug labels for use in treating obesity-related comorbidities and other illnesses. It comes as concerns remain around the drugs’ other possible side effects, such as muscle loss and suicidal thoughts, and U.S. authorities have pushed back against the high costs of the treatments.
Nevertheless, appetite for the treatments continues to balloon, with analysts estimating that the sector could be worth up to $200 billion by 2030.
Emily Field, head of European pharmaceuticals research at Barclays, said the weight loss market was likely to grow more “fragmented” over time as pharmaceutical companies target different segments, noting that treatments to counter muscle loss could be a good way to “differentiate.”
However, she noted that a company of Zealand Pharma’s size and scope would struggle to do so alone.
“It’s not something Zealand could even think about, manufacturing themselves. A lot of people who have owned it still own it, but are wondering if it’s going to get bought or not,” Field said over the phone.
Steensberg on Thursday ruled out growing speculation around a takeover, saying it’s “definitely not part of our plans.” But he noted that even with a significant $1 billion capital raise earlier this year, the company would need a partner.
“We have a clear ambition to continue into the next phase of our life as a partnering company,” Steensberg said. “We have to have a lot to offer and I think it’s a very attractive opportunity to partner with Zealand right now for a large pharma company.”
He added that partnership discussions are underway and likely to continue into the first half of next year.
Petrelintide and Dapiglutide will now progress to phase 2 trials on overweight and obese patients in late 2024 and the first half of 2025, respectively.
Credit: CNBC
