Muscle loss and protein needs in older adults
Team Metabolic Health
It’s not your imagination: it is harder to gain — or just maintain — muscle after middle age. Aging brings many changes to the body. One such change is muscle loss. Adults who don’t engage in regular strength training can lose 4 to 6 pounds of muscle per decade.
The technical term for age-related muscle loss is sarcopenia, and it affects nearly 50% of adults above the age of 80. While sarcopenia is a natural part of aging, it can impact quality of life by increasing the risk of frailty, disability, loss of independence, and even death.
To combat sarcopenia, you can build muscle through strength training. Building muscle requires protein, so when you’re aiming to increase muscle mass, your body needs more protein. Increasing dietary protein intake can support muscle repair and growth.
Getting more protein from your diet
The amount of protein a person should consume each day depends on factors such as height, weight, age, sex, and activity level. You can use this USDA calculator to find your daily recommended protein intake. For the average adult, the Recommended Dietary Allowance (RDA) of protein is 0.36 grams per pound of body weight. For a person who weighs 165 pounds, for example, that comes to 60 grams of protein per day.

Unfortunately, many older adults aren’t meeting their daily protein needs. A study published in the Journal of Nutrition, Health & Aging that looked at the diets of nearly 12,000 individuals ages 51 and older found that approximately 46% didn’t meet daily protein recommendations. Lower protein intake makes it more challenging to build muscle mass.
While consuming enough protein to support muscle gains is important for overall health, too much protein can also lead to health issues. Consuming very high amounts of protein per day — anything over 0.907 grams per pound; or about 150 grams per day for a 165-pound person — can be harmful. More than that can cause dehydration or aggravate kidney problems for individuals with pre-existing kidney conditions such as chronic kidney disease or a history of kidney stones.
A wide variety of foods, both plant- and meat-based, are high in protein. These include beans, peas, and lentils; nuts and seeds; lean meats; fish; dairy products; and soy products. Incorporating more of these foods into your diet is the easiest way to up your protein intake.
In addition to eating high-protein food sources, when you consume protein is also important. Experts recommend spreading protein consumption throughout the day, with good protein sources at each meal.
Can protein supplements help?
While the best source of protein in your diet is whole foods, some older adults who cannot get adequate protein through food alone may benefit from supplementation. To decide if you should add protein supplements to your diet, consult with your doctor.
Many people find protein supplements such as protein powders an attractive and easy solution to meeting their daily protein needs. Over-the-counter protein powder supplements have become increasingly popular in the United States and are a multibillion-dollar industry.
One reason may be that protein powders are convenient. They can be easily added to oatmeal or smoothies, or simply mixed into a glass of water. They come with convenient scoopers to help you see exactly how much protein you are adding. Always check the label to find the amount of protein per serving, as this varies by brand of supplement.
However, there are some concerns to be aware of when consuming protein supplements. Protein powders are classified as dietary supplements and are not regulated as strictly as food or medicine. In addition, the sugar content of protein powders can be vary depending on the brand; some brands may have as much as 23 grams per scoop. In addition, whey- or casein-based protein powders can cause digestive discomfort in some individuals.
Types of protein powders
There are three main types of protein powders: whey, casein, and plant-based protein powders. Both whey and casein are animal-based protein powders, made from dairy. Plant-based protein powders are usually a combination of protein derived from wheat, pea, hemp, or soy products.
Of the three, research suggests that whey protein is particularly effective for building muscle in older adults, more so than either plant-based proteins or casein.
For individuals who are avoiding dairy, plant-based protein powder options like soy isolate protein can also be beneficial. These generally have a lower amino acid profile and reduced bioavailability compared to animal-based proteins. Bioavailability is the measure of how much and how quickly a substance, such as a nutrient or drug, is absorbed and becomes available for use in the body. Vegan protein powders made from peas or brown rice are also suitable alternatives to dairy-based protein supplements.
The importance of resistance and strength training for preserving muscle mass
While protein is important for building muscle mass, it should be combined with strength training to combat sarcopenia. Research shows that supplementing the diet with protein plus a regimen of heavy resistance exercise leads to the most improvement in muscle mass and strength in healthy older adults. Together, the two approaches can significantly aid muscle growth in older adults.
Credit: health.harvard.edu
How — and why — to fit more fiber and fermented food into your meals
Team Metabolic Health
Fiber and fermented foods aid the gut microbiome, contributing to better health and mood.
An F may mean failure in school, but the letter earns high marks in your diet. The two biggest dietary Fs — fiber and fermented foods — are top priorities to help maintain healthy digestion, and they potentially offer much more. How can you fit these nutrients into meals? Can this help your overall health as well as gut health?

Fiber, fermented foods, and the gut microbiome
The gut microbiome is a composed of bacteria, viruses, fungi, and other microorganisms living in the colon (large intestine). What you eat, the air you breathe, where you live, and many other factors affect the makeup of the gut microbiome. Some experts think of it as a hidden organ because it has a role in many important functions of the body — for example, helping the immune system function optimally, reducing chronic inflammation, keeping intestinal cells healthy, and providing some essential micronutrients that may not be included in a regular diet.
Your gut communicates with your brain through pathways in the gut-brain axis. Changes in the gut microbiome have been linked with mood and mental health disorders, such as depression and anxiety. However, it’s not yet clear that these changes directly cause these types of problems.
Making Sense of Vitamins and Minerals
About half of all Americans routinely take dietary supplements. The most common ones are multivitamin and multimineral supplements. Making Sense of Vitamins and Minerals: Choosing the foods and nutrients you need to stay healthy explains the evidence behind the benefits and safety profiles of various vitamins and minerals. It also includes the recommended minimum and maximum amounts you should consume, as well as good food sources of each.
We do know that a healthy diet low in processed foods is key to a healthy gut microbiome. And increasing evidence suggests that fiber and fermented foods can play important parts here.
Fiber 101
Fiber’s main job is to make digestion smoother by softening and adding bulk to stool, making it pass quickly through the intestines.
But fiber has other benefits for your microbiome and overall health. A high-fiber diet helps keep body weight under control and lowers LDL (bad) cholesterol levels. Research has found that eating enough fiber reduces the risk of heart disease, type 2 diabetes, and some cancers.
What to know about fiber
There are two types of fiber: insoluble (which helps you feel full and encourages regular bowel movements) and soluble (which helps lower cholesterol and blood sugar). However, recent research suggests people should focus on the total amount of fiber in their diet, rather than type of fiber.
If you’re trying to add more foods with fiber to your diet, make sure you ease into new fiber-rich habits and drink plenty of water. Your digestive system must adapt slowly to avoid gas, bloating, diarrhea, and stomach cramps caused by eating too much too soon. Your body will gradually adjust to increasing fiber after a week or so.
How much fiber do you need?
The fiber formula is 14 grams for every 1,000 calories consumed. Your specific calorie intake can vary depending on your activity levels.
“But instead of tracking daily fiber, focus on adding more servings of fiber-rich foods to your diet,” says Eric Rimm, professor of epidemiology and nutrition at Harvard’s T.H. Chan School of Public Health.
Which foods are high in fiber?
Fruits, vegetables, legumes, nuts, seeds, and whole grains are all high in fiber. The Dietary Guidelines for Americans has a comprehensive list of fiber-rich foods and their calorie counts.
What about over-the-counter fiber supplements that come in capsules, powders that you mix with water, and chewable tablets? “If you have trouble eating enough fiber-rich foods, then these occasionally can be used, and there is no evidence they are harmful,” says Rimm. “But they should not serve as your primary source of dietary fiber.”
Fermented foods 101
Fermented foods contain both prebiotics — ingredients that create healthy changes in the microbiome — and beneficial live bacteria called probiotics. Both prebiotics and probiotics help maintain a healthy gut microbiome.
What to know about fermented foods
Besides helping with digestion and absorbing vital nutrients from food, a healthy gut supports your immune system to help fight infections and protect against inflammation. Some research suggests that certain probiotics help relieve symptoms of gut-related conditions like inflammatory bowel disease and irritable bowel syndrome, though not all experts agree with this.
Many foods that are fermented undergo lacto-fermentation, in which natural bacteria feed on the sugar and starch in the food, creating lactic acid. Not only does this process remove simple sugars, it creates various species of good bacteria, such as Lactobacillus or Bifidobacterium. (Keep in mind that some foods undergo steps that remove probiotics and other healthful microbes, as with beer or wine, or make them inactive, like baking and canning.)
The exact amounts and specific strains of bacteria in fermented foods vary depending on how they are made. In addition to probiotics, fermented foods may contain other valuable nutrients like enzymes, B vitamins, and omega-3 fatty acids.
How often should you eat fermented foods?
There is no recommended daily allowance for prebiotics or probiotics, so it is impossible to know precisely which fermented foods or quantities are best. The general guideline is to add more to your daily diet.
Which fermented foods should you choose?
Fermented foods have a range of tastes and textures because of the particular bacteria they produce during fermentation or that are added to foods. Yogurt is one of the most popular fermented foods (look for the words “live and active cultures” on the label). Still, many options are available if you are not a yogurt fan or want to expand your fermented choices. Kimchi, sauerkraut, kombucha, and pickles are a few examples.
As with fiber, probiotics are also marketed as over-the-counter supplements. However, like all dietary supplements, they do not require FDA approval, so there is no guarantee that the types of bacteria listed on a label can provide the promised benefits — or are even in the bottle. “Therefore, it is best to get your probiotics from fermented foods,” says Rimm.
Credit: health.harvard.edu
Ratan Tata’s legacy: Revolutionising cancer care in India, one hospital at a time
Team Metabolic Health
The Tata Group’s foray into healthcare began in 1941 with the establishment of the Tata Memorial Hospital in Mumbai.
- Ratan Tata and his team created a vast network of cancer care centers
- Tata knew that cancer treatment had to reach everyone
- He pushed to include these services in government insurance schemes
There is a reason why the titan Ratan Tata, who led over 30 companies in more than 100 countries, was never featured in the list of “billionaires” of the world or India.
Today, as we remember this “humble” tycoon for his significant contribution to philanthropy — long before India even heard of Bill Gates — his work in the field of cancer research in India is especially laudable.
Long before the world recognised the importance of philanthropy, Ratan Tata was quietly making a difference.
People pay homage to business leader Ratan Tata at NCPA lawns, in Mumbai. (Photo: PTI)
The Tata Group’s foray into healthcare began in 1941 with the establishment of the Tata Memorial Hospital in Mumbai. This was no ordinary hospital; it was a sanctuary of care for all, regardless of their background.
With this commitment, the foundation for a revolution in cancer treatment in India — unheard of at the time — was laid. The management of the hospital was handed over to the Ministry of Health in 1962.
Tata knew that cancer treatment had to reach everyone. The high costs meant many couldn’t afford the care. The Tata Memorial Hospital earned its name for providing free or economically viable treatments.
“Now, several Tata Memorial Centers have come up in Varanasi, Muzaffarpur, Punjab, and Visakhapatnam. The Tata Trust has a great legacy in creating facilities across the country to treat cancer patients. In 1992, bone marrow transplants were started by them in India. Nearly 1,000 cancer patients are seen there every day, and almost two-thirds are treated free of cost. This is a huge contribution by the Tata Trust and Tata family, which Ratan Tata continued to support, focusing on cancer care in the country. Their philanthropic contribution must be acknowledged,” said Dr. Shyam Aggarwal, head of medical oncology at Sir Ganga Ram Hospital, Delhi.
Tata Group Chairman Emeritus Ratan Tata speaks during an event, in Mumbai. (Photo: PTI)
In 2012, the Trusts launched the Tata Medical Center in Kolkata to address the high prevalence of cancer and the lack of suitable facilities in the eastern and northeastern regions.
The Tata Trusts are expanding their network to 20 hospitals across seven states: Andhra Pradesh, Assam, Jharkhand, Maharashtra, Uttar Pradesh, Odisha, and Gujarat.
Fast forward to 2017, when Ratan’s passion and dedication led to the launch of the ambitious Cancer Care Program through the Tata Trusts. This program introduced a groundbreaking concept: the “Distributed Cancer Care Model.” Imagine a world where cancer care is accessible, affordable, and of high quality—this was Ratan’s dream.
Ratan Tata knew his dream had to extend beyond Mumbai. Part of this project included the establishment of new cancer hospitals in Assam and Uttar Pradesh. State governments were also further assisted by Ratan Tata in setting up cancer hospitals and treatment facilities in smaller towns and cities.
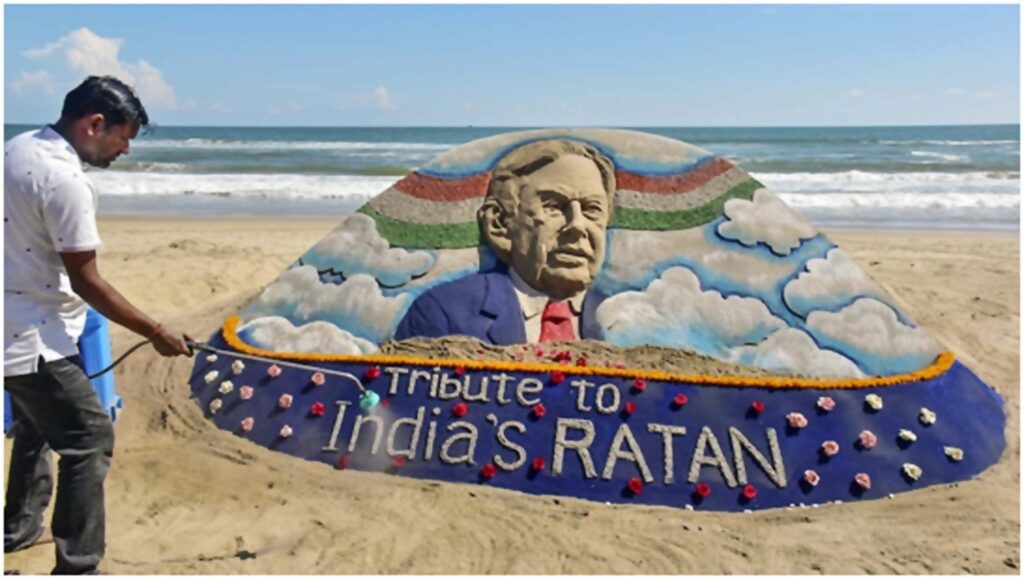
Puri: Sand artist Sudarsan Pattnaik creates a sand sculpture to pay tribute to Ratan Tata at Puri beach in Odisha, Thursday, Oct. 10, 2024. (PTI Photo)
Ratan Tata was acutely aware of the statistics: over 70% of cancer cases in India were diagnosed at late stages. With this knowledge, he set an ambitious goal—to reverse that ratio from 30:70 to 70:30.
To bring this dream to life, Ratan and his team created a vast network of cancer care centers, daycare facilities, and screening kiosks. Knowing that financial barriers often kept people from seeking treatment, he pushed to include these services in government insurance schemes, transforming the landscape of cancer care in India.
Recently, the Tata Institute in Mumbai claimed to have discovered a treatment that can prevent cancer from recurring with a tablet costing just ₹100.
Researchers and doctors at the institute worked for 10 years and have now developed a tablet they claim can prevent the recurrence of cancer and reduce the side effects of treatments like radiation and chemotherapy by almost 50%.
Assam Chief Minister Himanta Biswa Sarma mourned Ratan Tata’s passing, highlighting his transformative impact on the state through initiatives in cancer care and the establishment of a semiconductor industry.
Tata’s commitment to Assam was demonstrated through several key initiatives, including the establishment of the Assam Cancer Care Foundation, which aims to enhance healthcare services in the state.
According to the latest IIFL Wealth Hurun India Rich List of 2022, Ratan Tata ranked 421st, with a net worth of approximately Rs 3,800 crore. However, the Tata Group companies have bequeathed their assets to the Tata Trusts, which hold a two-thirds stake in Tata Sons.
Approximately 60% of the dividends from Tata Sons are allocated to charitable endeavors, according to available information.

Tata’s commitment to Assam was demonstrated through several key initiatives. (Photo: India Today)
“As we remember Ratan Tata, his work in revolutionizing cancer care stands as a testament to his vision, compassion, and commitment to improving the lives of millions,” said Dr. Mohit Saxena, Consultant and HOD Medical Oncology at Manipal Hospital, Gurugram.
He added, “Under Tata’s leadership, the Trusts launched impactful awareness campaigns like ‘Kaise Ka Cancer’ and ‘Gaanth Pe Dhyaan.’ The program’s comprehensive approach included community-based cancer screening, training healthcare providers, tobacco control initiatives, and leveraging technology for better patient management.”
As we reflect on Ratan Tata’s remarkable journey, we see a life dedicated to compassion and change. Without the Tata legacy, the advancement of cancer treatment for Indians, by Indians, would perhaps be a distant and very expensive dream.
Credit: India Today
The golden era of GLP-1 drugs: Where we are and what comes next
Team Metabolic Health
Glucagon-like peptide 1 (GLP-1) receptor agonists (RAs) are entero-pancreatic hormone-based treatments first approved in 2005 for type 2 diabetes (T2D). They are now commonly prescribed for weight loss and reduction of atherosclerotic cardiovascular (CV) risk in patients with T2D.
The health benefits and market success of GLP-1 drugs are a hot topic in today’s pharmaceutical landscape. According to a MarketWatch report from February 2024, the global GLP-1 market is expected to reach $471 billion by 2032. As of February 2024, there were 15 GLP-1 medications approved by the FDA for glycemic and weight control, and more were already in development.

imyskin via Getty Images
More than one billion people worldwide are living with obesity, which puts them at risk of major health complications, such as T2D, high blood pressure, heart disease, stroke, metabolic syndrome, fatty liver diseases, some cancers, kidney disease, breathing problems, and sleep apnea. Most of these diseases are interrelated, with glycemic control and weight loss being a major factor in improving the overall health of sufferers.
We are in an era where combinations of entero-pancreatic hormones can deliver significant weight loss, and patients are experiencing health benefits well beyond blood sugar management and weight loss.
“As we learn more about GLP-1 RAs, we realize that they target many organ systems, including the pancreas, the stomach, brain, heart, kidneys, immune system (due to reduced inflammation), skeletal muscle, control of metabolism of both white and brown adipose tissue, and positive effect in fatty liver disease (nonalcoholic fatty liver disease and steatohepatitis; MAFLD and MASH),” says Dr. Gaetano Morelli, Chief Medical Officer at Altasciences.
What GLP-1 is and how receptor agonists work
Dr. Gaetano Morelli explains, “GLP-1 is a hormone called an incretin or gut peptide released by endocrine cells in the small intestine in response to nutrient ingestion, mainly glucose and fat.”
Clinical data on GLP-1 RAs
GLP-1 RAs mimic the action of endogenous GLP-1 and, in head-to-head clinical studies, have demonstrated that all GLP-1 RAs are effective at reducing A1C levels. These initial pivotal studies that led to the first wave of GLP-1 RAs demonstrated that they work in several ways, including stimulating insulin release, slowing digestion, reducing appetite, and inhibiting glucagon release.
A guidance from the U.S. FDA (draft updated in March 2020) requires data on cardiovascular events in new T2D drug development programs. As a result, dedicated cardiovascular safety trials were implemented. Many demonstrated beneficial effects of GLP-1 RAs on the heart and kidneys in patients with T2D (with and without preexisting conditions), with those effects thought to be largely independent of glucose-lowering.
More recently, pharmaceutical companies have sponsored large cardiovascular outcomes trials (CVOTs) to assess the beneficial effects of GLP-1 RAs on the cardiovascular system in patients with T2D, with encouraging results.
What comes next
Looking to the next generation of clinical trials for obesity treatments, we see combinations of GLP-1 RAs with other entero-pancreatic hormones with complementary actions and/or synergistic potential (such as glucose-dependent insulinotropic polypeptide (GIP), glucagon, and amylin) to enhance the weight loss and cardiometabolic benefits of GLP-1 RAs. There are currently more than 140 of such compounds in development. Drug developers are also investigating the potential for longer-lasting injections.
Oral formulations are another future enhancement for GLP-1 RA medicines, with several pill forms in development. Various physiological barriers, such as mucus, intestinal, and enzymatic barriers, interfere with the oral delivery or absorption of protein and peptide-based therapeutics. Thus, novel approaches such as nanocarriers, site-specific, and stimuli-specific delivery, are being used to improve the success of oral GLP-1 RAs.
Sources indicate that newer GLP-1s have fewer side effects, although the most common gastrointestinal issues (nausea, vomiting, and diarrhea) may continue. Loss of muscle mass, often associated with rapid weight loss, is another potential side effect being investigated. Long-term side effects of GLP-1 usage are currently unknown, and researchers are accumulating data as this therapeutic area continues to boom.
“Promising programs have been halted due to challenges with side effect profiles and drug interactions, and diligent, expert program development will be critical as we move into the next generations of these important therapeutics,” says Dr. Morelli. “Developing newer and better GLP-1 RAs is a crucial contribution to global human health, and it is a field we at Altasciences are proud to be advancing.”
Credit: biopharmadive.com
Is the portfolio diet the best diet ever?
Maybe — but that could be the wrong question.
Team Metabolic Health
What we eat can play a pivotal role in warding off — or treating — disease and enhancing quality of life. You may already believe this, and certainly mounting evidence supports that idea. But on the cluttered shelf of diets claiming top health benefits, which one ranks as the absolute best?
That’s a trick question. In fact, there is no single best diet. A good diet for me may be different from what’s best for you. And for either of us, there may be several good choices with no clear winner.
How can you choose the right diet for you?
When thinking about what diet might be best for you, ask yourself:
What goals are most important? A goal might be weight loss, improved health, avoiding disease, or something else.
How do you define “best”? For some people, best means the diet with the highest number of health benefits. For others, it may focus on one specific health benefit, such as lowering cholesterol. Still other people may prefer a diet that delivers the greatest benefit for the lowest cost. Or a diet that is healthy and also easy to stick with.
What health problems do you have? One diet may have an advantage over another depending on whether you have cancer, cardiovascular disease, diabetes, or none of these.
Which foods do you like best? Your tastes, culture, and location may shape your dietary preferences, and powerfully affect how likely you are to stick with a specific diet.
Which diets are high in health benefits?
Two very well studied diets demonstrate clear benefit, including lowering risk for heart disease and stroke and reducing high blood pressure: the Mediterranean diet and the DASH diet.

But the portfolio diet may be as good as or better than these plans, at least for combatting cardiovascular disease that contributes to clogged blood vessels, heart attacks, and stroke. What? You’ve never heard of the portfolio diet? You’re not alone.
What is the portfolio diet?
Just as a financial advisor may recommend having a diverse investment portfolio — not just stocks, not just bonds — the portfolio diet follows suit. This largely plant-based diet focuses on diverse foods and food groups proven to lower harmful blood lipids, including LDL (so-called bad cholesterol) and triglycerides.
If you choose to follow this eating pattern, you simply need to learn which foods have a healthy effect on blood lipids and choose them in place of other foods. For some people, this only requires small tweaks to embrace certain foods while downplaying other choices. Or it may call for a bigger upheaval of longtime eating patterns.
Which foods are encouraged in the portfolio diet?
Below are the basics. Eating more of these foods regularly may help lower levels of harmful blood lipids:
Credit: health.harvard.edu
Essential Guide to GLP-1 Agonists for Weight Loss
Team Metabolic Health
Essential Guide to GLP-1 Agonists for Weight Loss: It was originally thought that GLP-1 agonists could help people with type 2 diabetes, but now they are known to help people lose weight very effectively. These medicines work like the hormone glucagon-like peptide-1, which helps keep blood sugar and hunger levels in check.
GLP-1 agonists can help people lose a lot of weight, even if they don’t have diabetes, by making them feel full and lowering the amount of food they eat. Options like semaglutide and liraglutide have shown promise in clinical studies.
Anyone thinking about using them to lose weight needs to know about their benefits, possible side effects, and the right way to use them.
What Are GLP-1 Agonists?
GLP-1 agonists, also known as glucagon-like peptide-1 receptor agonists, are a group of drugs that were first created to treat type 2 diabetes. These drugs work like the hormone GLP-1, which is found in the body and is very important for controlling blood sugar and hunger.
GLP-1 agonists help lower blood sugar levels by making insulin work better and stopping glucagon from working. They also slow down the emptying of the stomach, which can help you feel fuller and eat less, which is especially good for weight loss.
There are a number of GLP-1 agonists on the market right now, such as semaglutide (marketed as Ozempic and Wegovy), liraglutide (Saxenda), and dulaglutide (Trulicity). Although these medicines have mostly been used to treat diabetes, studies have shown that they can also help people who don’t have diabetes lose a lot of weight.
In fact, new study shows that they can help people lose weight, which makes them an important tool in the fight against obesity.GLP-1 agonists are especially good for helping you lose weight.
People who take these drugs can lose 10 to 15 percent of their body weight in a year, and some people lose even more. People who lose weight often also see changes in their metabolic health, such as lower blood sugar, better cholesterol levels, and lower blood pressure.
GLP-1 agonists are a good choice for people who are overweight or obese and are having health problems because they help you lose weight in a healthy way.
Benefits and Considerations
One great thing about GLP-1 agonists is that they can make you feel less hungry and cut down on your wants. By affecting the brain’s hunger control areas, these drugs can help people feel fuller for longer, which can make it easier to stick to a low-calorie diet.
This can be especially helpful for people who have a hard time controlling how much they eat. GLP-1 agonists also help you lose weight slowly, which helps you keep your lean muscle mass, which is important for keeping your metabolism healthy.
But even though GLP-1 agonists have a lot of benefits, they can also have some bad affects. Some of the most common side effects are feeling sick, throwing up, having diarrhea, and stomach pain, especially when you first start taking the medicine. Most of the time, these signs get better as the body gets used to them.
People who are thinking about taking GLP-1 agonists should talk to a doctor or nurse about the possible side effects and find out if these drugs are right for them. Also, GLP-1 agonists are usually recommended as part of a complete weight loss plan that includes changes to your diet and more exercise.
Another thing to think about is how much GLP-1 agonists cost and how easy it is to get them. These medicines can be pricey, and insurance plans may not cover them all. People should check with their insurance company and look into patient aid programs if the cost is a problem.
In addition, GLP-1 agonists are given through injection, which some people may not like. Those who are thinking about getting regular injections need to know how much time and effort they will take.
To sum up, GLP-1 agonists look like a good way to lose weight, especially for people who are overweight. They are useful for managing weight because they make you feel fuller, help you lose weight in a healthy way, and improve the health of your metabolism.
But people who are thinking about using these medicines should compare the benefits to the risks and costs. Talking to a doctor or nurse is important to make sure that your weight loss plan is safe, successful, and fits your health needs and goals.
As long as obesity is a major health problem around the world, GLP-1 agonists will likely play a bigger part in treatment plans. More study is needed to find out what their long-term effects are and if they can be used for things other than weight loss and diabetes management.
People who want to lose weight and keep it off may find that GLP-1 agonists are a useful addition to their toolbox. They may give them hope for long-term weight loss and better health generally.
Credit: ahrcc.in
Sharp rise in vaping among young adult non-smokers
Team Metabolic Health
The number of adults in England to have started vaping despite never having been regular smokers has reached one million, scientists estimate.
This is a sharp increase on 2020, with disposable vapes having been available since 2021.
The rise is driven mostly by young adults – with about one out of every seven 18-24-year-olds who never regularly smoked now using e-cigarettes.
While some may have benefited by taking up vapes instead of traditional cigarettes – the trend could be worrying, experts say.

Many people who take up vaping have never been regular smokers. (Getty Images)
‘Less harmful’
Lead researcher, Dr Sarah Jackson, at University College London (UCL), said the public-health impact of the “substantial rise” in vaping among people who have never regularly smoked depended on what they would otherwise be doing.
“It is likely that some would have smoked if vaping were not an available option,” she said.
“In this case, vaping is clearly less harmful.
“However, for those who would not have gone on to smoke, vaping regularly over a sustained period poses more risk than not vaping.”
How dangerous is vaping?
Researchers looked at surveys of about 150,000 adults in England between 2016 and 2024.
Respondents agreeing with the statement: “I have never been a smoker – ie smoked for a year or more,” were counted as “never regular smokers”.
And between 2016 and 2020, only 0.5% of these vaped.
But by April 2024, this had risen to 3.5%, with more than half aged between 18 and 24.
Over the last few years, these “never regular smokers” who took up vapes tended to be younger, more were women, and more were drinking at increasing levels, than in the past, researchers say.
The study, published in the journal Lancet Public Health journal and funded by charity Cancer Research UK, also found overall vaping figures among adults were levelling off.
Disposable vapes to be banned for child health
Senior researcher, Prof Jamie Brown, at UCL, said: “These findings are a reminder that action is required to try to minimise vaping among young people who have never previously smoked.
“However, a balancing act is required to avoid deterring smokers from using e-cigarettes to quit.”
Current government plans to ban disposable vapes were unlikely to be the solution, Prof Brown suggested, as popular brands had already launched reusable products that looked and costed almost the same.
“A sensible next step would be to introduce stricter regulation around product appearance, packaging and marketing,” he added
Steep fall in young smokers in past decade
Hazel Cheeseman, chief executive of campaign group Action on Smoking and Health (Ash) said the findings could be a cause for concern and suggested focusing on reducing the appeal of vapes would be the best way to limit the use of vapes in non-smokers.
“The aggressive marketing of products to young people means the government urgently needs to bring back the Tobacco and Vapes Bill, to regulate vape flavours, marketing and branding,” she said.
Peter Hajek, professor of clinical psychology, at Queen Mary University of London, said: “The just-released figures from the Office for National Statistics show that UK smoking prevalence is under 12%, an all-time low.
“If much less risky alternatives are allowed to continue to compete with cigarettes, smoking – and heart disease, lung disease and cancers that it causes – will continue to decline as well.
“The UK and USA, which allow vaping, have seen significantly faster declines in cigarette sales and in smoking among young and low-income people than Australia, which bans vaping. “
Credit: BBC News
England’s NHS to offer Lilly’s weight-loss drug to some patients
Team Metabolic Health
England’s National Health Services will offer Eli Lilly’s (LLY.N), opens new tab weight-loss drug to nearly a quarter million people as part of a three-year plan, the country’s drugs cost regulator said on Thursday.
The drug, called Mounjaro in the UK and Zepbound in the U.S., would be initially offered to obese people with at least three weight-related health conditions, the National Institute for Health and Care Excellence said.
The conditions are hypertension, sleep apnea, cardiovascular disorders and unhealthy levels of lipids like cholesterol.
As part of a phased rollout, the drug would then be offered to people with two of the conditions and then to those with just one.
The plans have been described in an application from the NHS to UK’s National Institute for Health and Care Excellence.
An injection pen of Zepbound, Eli Lilly’s weight loss drug, is displayed in New York City, U.S., December 11, 2023. REUTERS/Brendan McDermid
As part of the plan, the NHS will test several new services to offer the drug, including digital technologies, and will select the most cost-effective one.
NHS plans to offer the drug as part of a “wraparound package”, which will include diet and exercise support through primary or secondary care clinics.
“This is no small task for the NHS, and it will be difficult to provide the level of wraparound care seen in patients who took part in the clinical trial,” said Simon Cork, a physiology lecturer at Anglia Ruskin University.
About 64% of adults are either overweight or living with obesity in England, according to a national survey.
Rival Novo Nordisk’s (NOVOb.CO), opens new tab Wegovy made its weight-loss debut in the UK last year and was also approved in July to reduce risk of serious heart problems or strokes in overweight and obese adults.
The NHS currently offers Wegovy through specialist weight management services.
Credit: Reuters
You’re Due for a Colonoscopy, but What if You Don’t Want It?
Team Metabolic Health
Doctors can provide alternative forms of screening for colon and rectal cancer but sometimes have a good reason to stick with the colonoscope.
This year about 53,000 Americans are expected to die from colon or rectal cancer. Doctors say most people should start getting screened at age 45. Yet many who are eligible skip testing.
When most people in this country think of colon cancer screening, they think of colonoscopies, which let doctors examine the colon but can be inconvenient. Yet there are other equally acceptable options for screening.
If more people knew about other kinds of colorectal cancer testing, some experts hope, perhaps some who put off colonoscopies would be screened and deaths from colon cancer could be avoided.

A colonoscopy will find 95 percent of the time if cancer is present, but other tests that rely on fecal samples are not always as accurate .Credit: iStock/Getty Images Plus
Here’s what you need to know about colonoscopies and fecal tests, which to ask for, and why your doctor might be recommending one over the other.
How do colonoscopies and fecal tests work?
Colonoscopies are widely used, but there is another option available: fecal tests.
Both types of test attempt to find cancers and large polyps — growths on the wall of the colon — that occasionally turn into cancers. Cancers that are found early often can be cured when doctors simply cut them out. Finding and removing polyps can also prevent cancers.
Colonoscopies start with a patient’s taking strong laxatives to empty the colon. On the day of the test, the patient is sedated. Then, a doctor inserts a colonoscope — a flexible tube with a video camera at the end — into the rectum and colon and looks for polyps and cancers to remove. The doctor may also take samples for study in a lab.
If no polyps or cancers are found, the average patient can wait 10 years before having another colonoscopy.
Fecal tests can be done at home. Patients collect a stool sample and mail it to or drop it off at a testing lab.
One option is the fecal immunochemical test, or FIT, which should be repeated annually. A lab analyzes the sample for traces of blood, which can indicate a polyp or cancer. Large polyps and colon cancers sporadically ooze small amounts of blood. If blood is detected, the patient must have a colonoscopy.
Another more complex fecal test is Cologuard, repeated every three years. It looks for blood in stool and also for abnormal DNA from large polyps and colon cancers. Like the FIT test, Cologuard must be followed by a colonoscopy if blood or abnormal DNA are present.
Which option actually works better?
That depends on what is meant by “better.”
One measure is how often a test finds large polyps.
If a person who has a large polyp has a colonoscopy, the test will detect it 95 percent of the time. If that person has a Cologuard test, there is a 42 percent chance that it will be positive because of the polyp. If the person has a FIT test, there is about a 22 percent chance it will be positive.
Another measure is how likely the test is to find cancers when they are present.
Colonoscopies find 95 percent. A one-time Cologuard test will be positive 94 percent of the time if a cancer is present, and a FIT test will be positive 74 percent of the time.
The ultimate goal, though, is preventing colon cancer deaths. For now, no one really knows which test performs better. One large clinical trial by the Department of Veterans Affairs is comparing the number of colon cancer deaths among 50,000 patients randomly assigned to have a colonoscopy or an annual FIT test and followed for 10 years.
Results are expected in 2027 or 2028.
While those studies are continuing, other studies have compared a screening test with no test.
One study found that after 30 years, people who had fecal tests had a 33 percent lower death rate from colon cancer than people who were not screened. The death rate fell to 2 percent, from 3 percent.
A 10-year European study of colonoscopy found a 30 percent reduction in the risk of getting colon cancer. It was 0.84 percent in a group that had colonoscopies and 1.22 percent in a group that was not screened. There was no difference in the risk of dying from colon cancer.
Whether the reduction in the risk of getting colon cancer is worth a potential risk of injury during the surgery is “in the eye of the beholder,” said Dr. Michael Bretthauer, a gastroenterologist at the University of Oslo who led the study.
Can I ask my doctor for a fecal test if I prefer it to a colonoscopy?
Of course — if you are of average risk, meaning no family history of colon cancer and no genetic condition that predisposes to colon cancer. If you are at a higher risk, your doctor is likely to advise a colonoscopy.
When patients of average risk ask Dr. David Lieberman, a gastroenterologist at Oregon Health and Science University, if they can skip the colonoscopy, he explains that a fecal test and a colonoscopy accomplish different things. Fecal tests are likely to find cancers when they are early enough to be cured. But he says those tests are not so good at finding precancerous polyps. While the hope is that, repeated over time, the fecal tests will find polyps, colonoscopies find both with a single test.
Hearing that, he said, most patients decide they want colonoscopies.
Credit: The New York Times
Why is this ‘miracle’ weight-loss drug still not available in NZ?
Team Metabolic Health
It has been labelled a “miracle drug” and has become a trending hashtag on social media, with celebrities like Sharon Osbourne, Rebel Wilson and US comedian Tracy Morgan touting its weight-loss benefits.
Yet more than six years after Ozempic first came onto the global market, Kiwis are still not able to get their hands on a drug many claim is the answer to shedding stubborn kilos for those who have tried nearly every other weight-loss strategy.
Peter Shepherd, a molecular medicine professor at Auckland University and expert in diabetes and obesity, says the long-term impact of Ozempic “could be huge” for New Zealanders.
“We can argue till the cows come home about whether people should lose weight themselves the so-called ‘hard way’, but the reality is, for many, it is just not happening. So either we sit here and ignore [the obesity problem], or we do something about it.”
Ozempic mimics a hormone called GLP-1, which helps lower blood sugar and promotes a feeling of fullness, making it easier for users to cut out snacking.
Shepherd is supportive of the drug being funded in New Zealand as he believes the greater health benefits of a decline in obesity – like a decrease in cardiovascular disease, less kidney dialysis and even improved mental health – would be a worthy return on investment.

The injectable drug Ozempic has been approved for the treatment of type-2 diabetes in New Zealand, but it is not sold here currently. (File photo) ASSOCIATED PRESS
‘Life-changing’ for one Kiwi
Since Ozempic is not sold in New Zealand, only a handful of Kiwis have been able to use the drug.
One of them is Wellington company director Finlay Thompson. For him, it was “life-changing”.
He enrolled in an international clinical trial in April last year, which aimed to research the effects of taking Ozempic along with another non-weight loss drug.
Weighing 138kg, Thompson says he struggled with his weight for years and unsuccessfully tried every kind of diet and exercise programme under the sun to shift it. When he got the chance to take Ozempic, he jumped at it.
And the weight started falling off.
“It is hard to explain, but it changed the way I felt about food. Before the trial, I was basically thinking about food the whole time, but when I was on Ozempic, I no longer felt like that. It all went away.
“Suddenly when I went to functions or dinners, I ate and became quite full, where before I could eat and eat and never really feel full. It was quite odd.”
Thompson lost 30kg before his weight plateaued at 108kg. He says the trial required him to stop taking Ozempic about a month ago, with researchers now studying the effects after patients stop taking the drug. So far he hasn’t regained any of the weight he lost.
He experienced some side effects while taking the drug, “mostly gut-related”, but says these were nothing compared to the health impacts of being overweight.
Thompson says while he would still like to lose another 8kg or 9kg, the 30kg loss is “enough” to have changed his life.
“At 138kg, that’s quite a debilitating state to be in. Everything is just easier now, even just walking around. Imagine walking around with a heavy 30kg bag and then just putting it down. It makes a massive difference.”
The drug comes with the risk of side effects like nausea, diarrhoea and constipation, but serious side effects are rare, Shepherd says.
“It’s not the final solution. There will be learnings as we go on that will lead us to, say, identify the people for whom this is the right drug or limit the side effects. It is very exciting, but we will learn along the way.”
Diabetes drug used for weight loss
Ozempic, the trade name for a semaglutide injection, was developed to treat type 2-diabetes. Semaglutide works by mimicking a hormone called GLP-1, which helps lower blood sugar and promotes a feeling of fullness.
Ozempic is changing eating habits, and food companies are taking notice
“GLP-1 was found to improve the way we produce insulin, and so the idea was to develop this as an anti-diabetic drug to improve the body’s ability to release the right amount of insulin,” Shepherd says.
“Then it was realised that when you had higher doses of this GLP-1, people started to lose a bit of weight. And so what they did was develop chemical ways to make the drug last longer in your blood.
“So what Ozempic is is basically a modified human hormone that helps treat diabetes and also has weight-loss effects.”
Ozempic is made by Danish pharmaceutical company Novo Nordisk, the same company behind popular weight-loss drug Wegovy, which is also a semaglutide injection.
Its direct competitor is American pharmaceutical company Eli Lilly, which sells a similar drug under the brand names Mounjaro, for diabetes, and Zepbound, for weight loss.
Shepherd explains Ozempic is not the same as Saxenda, an anti-diabetic prescription medication currently available and used for weight loss in New Zealand. Saxenda is not funded.
Saxenda is a form of liraglutide rather than semaglutide, and Shepherd says although it is similar, “semaglutide hangs around longer and so it is more effective”.
Ozempic does not work for everyone and some find the side effects unbearable.
Medsafe announced in June last year it has approved Ozempic for the treatment of type 2 diabetes. Despite the regulatory approval, Novo Nordisk has still not launched the product here.
Professor Peter Shepherd, a molecular medicine professor at Auckland University and expert in diabetes and obesity, is supportive of Ozempic being funded as the greater health benefits of a decline in obesity would be a worthy return on investment.
A spokesperson for the company says it is “exploring options to provide access to Ozempic for people living with type-2 diabetes in New Zealand”, but did not respond to a question about when the drug will be available.
Information on the company website states that “increased demand for Ozempic”, coupled with “capacity constraints at some of the manufacturing sites”, have led to shortages of the drug, which are expected to continue throughout 2024.
“It is uncertain when supplies will be sufficient to fully meet current demand.”
The price tag
While there is no way to know what the sale price will be when Ozempic is finally launched in New Zealand, it could be similar to that in Australia, where a month-long supply costs about A$140 (about $150) if not funded via Australia’s Pharmaceutical Benefits Schedule.
This is significantly cheaper than in the US, where Ozempic retails for an average of US$936 a month – about $1480.
Saxenda currently sells in New Zealand for about $480 for a month’s supply.
Associate Professor Hesham Al-Sallami, a University of Otago expert on diabetes and obesity medication, believes if Ozempic or similar medicines were funded in New Zealand, it would take considerable pressure off the hospital system.
“If Ozempic can help patients lose weight, this could reduce the number of people getting type-2 diabetes in the first place,” Al-Sallami said in an article published on the university website last year.
“If this drug is made accessible in New Zealand as a weight-loss medication and is funded by Pharmac for that use as well, this could have considerably positive health outcomes for the country, taking pressure off the hospital system by reducing things like heart attacks and strokes.”
A Ministry of Health spokesperson says while Ozempic has not been approved as a treatment specifically for weight-loss in New Zealand (Novo Nordisk has not applied for this approval), Ozempic may still be prescribed by a medical practitioner for treating obesity.
“In these cases, the prescriber has the responsibility to ensure all treatment meets ethical and professional standards.
“If the use of a medicine is unapproved, the consumer should be advised, and the prescriber should discuss the evidence to support the use and any potential associated safety concerns.”
It is unclear whether any New Zealanders are importing Ozempic from overseas for personal use.
While it is legally possible to do so, the process is cumbersome and might prove difficult given there is a global shortage of Ozempic.
In August, the Australian Therapeutic Goods Administration reviewed the shortage of the drug and advised clinicians not to start new patients on Ozempic unless absolutely needed, and consider changing patients already on Ozempic to an alternative “as continuous supply cannot be guaranteed”.
The UK Department of Health and Social Care has banned the export of all forms of semaglutide and, according to media reports, many other European countries are considering imposing the same ban.
Another complication in importing Ozempic is the fact that it should be kept refrigerated at 2C to 8C.
A Medsafe spokesperson says Kiwis are allowed to import Ozempic from overseas if they have the authority from a New Zealand-registered authorised prescriber (usually their GP).
“Medsafe continues to warn that ordering medicines over the internet can be a risky business as a site may be located overseas and not have the credentials it claims to have,” the spokesperson says.
“In particular, ordering medicines is fraught with problems exposing the purchaser to poor quality and possibly counterfeit products from potentially illegal sources.”
Credit: thepress.co.nz
Lilly’s weight-loss drug removed from FDA’s shortage list
Team Metabolic Health
The U.S. Food and Drug Administration removed Eli Lilly’s (LLY.N), opens new tab blockbuster weight-loss and diabetes drugs from its shortage list late on Wednesday, likely piling pressure on firms selling cheaper versions known as compounded drugs.
Diabetes treatment Mounjaro has been on the health regulator’s shortage list since late 2022, while weight-loss drug Zepbound was added in April as demand far outstripped supply.
The limited supply for Lilly’s drugs, as well as rivals from Novo Nordisk (NOVOb.CO), opens new tab, had led to a boom in demand for compounded medicines, or custom-made treatments created by combining, mixing, or altering drug ingredients.
Federal regulations allow compounded versions to be sold to meet demand if a drug is in shortage. Outside of a shortage, compounders cannot make the drugs “regularly or in inordinate amounts.”

An injection pen of Zepbound, Eli Lilly’s weight loss drug, is displayed in New York City, U.S., December 11, 2023. REUTERS/Brendan McDermid/File
“This essentially precludes compounded tirzepatide from being produced commercially,” BMO Capital Markets analyst Evan Seigerman said in a research note, referring to the chemical name for Lilly’s drugs.
Novo Nordisk’s treatments still appeared on the FDA’s shortage list on Thursday. Lilly has started selling vials of the lowest dose of Zepbound in U.S. through its direct-to-consumer website to improve availability and combat the rise in popularity of compounded versions.
BMO’s Seigerman had earlier said that if the additional supply in vials gets Lilly’s drugs removed from the shortage list, it would allow the drugmaker to more easily sue those selling compounded versions of Zepbound.
Shares of Hims & Hers Health (HIMS.N), opens new tab, which offers compounded versions of Novo’s treatments, fell 7% to $17.62 in premarket trading.
Lilly is investing billions of dollars to boost production amid surging demand for Mounjaro and Zepbound. Novo, which makes rival drugs Ozempic and Wegovy, is also ramping up supply to meet unprecedented demand.
Credit: Reuters
Spiralling obesity costs could be solved by Ozempic and other weight-loss drugs
Team Metabolic Health
Weight loss drugs are effective and could help solve the obesity epidemic. The economic case for weight loss drugs is strong. Yet there are caveats: governments should prioritise prevention first and foremost, while access to medicines containing semaglutide should be safeguarded as there is a global shortage
Weight loss drugs can help solve the obesity epidemic
The active ingredient in weight loss drugs (semaglutide) acts like glucagon-like peptide 1 (GLP-1). By connecting to your GLP-1 receptors, weight loss drugs make you feel less hungry and fuller, helping people to lose weight.
Weight loss drugs offer a less expensive and less invasive alternative to other obesity treatments like gastric bypass surgery. This is fundamentally a good thing, as obesity rates have risen sharply over the past few decades. In fact, there are currently more people overweight than malnourished worldwide. Weight loss drugs can help reverse this trend.
Obesity carries significant societal costs. It is linked to health issues such as cardiovascular diseases, joint problems, and diabetes, all of which are costly to treat. Additionally, the Organisation for Economic Co-operation and Development (OECD) has shown that obesity reduces labour force participation and lowers productivity. Obesity also negatively impacts physical and mental well-being, adding to societal costs.
In short, there is a clear demand for weight loss drugs and they can help solve a real problem that bears significant societal costs.
How high are the societal costs of obesity?
Costs from obesity can be categorised into three types: healthcare, economic, and private costs. Healthcare costs are medical expenditures that stem from the diagnosis and treatment of other diseases caused by obesity, such as diabetes. Economic costs, on the other hand, are costs that stem from lower productivity. People with obesity are sick more often and longer than employees with a normal Body Mass Index (BMI), which means that their labour productivity is lower. Private costs are costs incurred by the individuals themselves. These are costs such as informal care and additional household expenditures, but also costs related to health-related quality of life such as self-care, pain and depression or anxiety.
These costs differ per country of course: healthcare and indirect costs are not the same across the globe. Yet, what is similar is that the societal costs of obesity mainly stem from the loss of productivity (i.e. more frequent sick days), and less so from healthcare costs. So much so that in the US and the Netherlands, three-quarters of the costs of obesity are not healthcare-related, but mainly caused by a productivity loss. However, the share of healthcare costs does increase as people become more overweight. In the US, for instance, adults with class 1 obesity experienced 68.4% higher healthcare costs than people with normal weight, whereas people with class 3 obesity had 233.6% higher costs. As people’s BMI increases, healthcare costs rise at a faster rate compared to non-healthcare costs.
How do societal costs of obesity compare to the costs of weight loss drugs?
As there are high societal costs associated with obesity, there is a strong economic incentive to solve the obesity epidemic. Yet, weight loss drugs are not free either. The costs of these drugs are one of the reasons that the Dutch Care Institute recently argued that Wegovy should not be covered under basic health care insurance. The Institute argued that the costs could amount to €1.3bn annually, which would be a significant dent in the Dutch healthcare budget of €95bn.
So, how do the prices of a year’s supply of Novo Nordisk’s Ozempic and Wegovy compare to the costs of additional healthcare? In Germany and the Netherlands, there is a clear economic case for weight loss drugs, as the annual costs of Ozempic are lower than the costs of additional healthcare and the costs of Wegovy are slightly higher. In the US, however, prices of weight loss drugs outweigh the yearly additional medical costs.
The US generally pays higher prices for both on-patent and generic drugs, which is also the case for Ozempic and Wegovy, but also for other weight loss drugs Rybelsus and Mounjaro. Both these drugs have similar price points as Ozempic in the US, and cost roughly fivefold (Rybelsus) and threefold (Mounjaro) more than they cost in Europe.
In addition, we have chosen to only look at additional healthcare costs, as the payment for weight loss drugs would likely come from healthcare budgets. Yet, as we know healthcare costs are roughly 25% of societal costs of obesity, so in reality the economics of weight loss drugs are better still. Moreover, the prices of the weight loss drugs are based on list prices, which can be higher than the actual prices paid, as healthcare insurers and providers can negotiate.
Long-term economic effects of weight loss drugs are uncertain
However, the long-term effects of weight loss drugs are still uncertain. The most poignant question is whether weight loss results are sustainable when the use of weight loss drugs is tapered off. In short, is weight loss a short- or long-term result?
If weight loss results are sustainable then the economic case for weight loss drugs becomes stronger. This likely means less medical costs later in the life of patients when costs of obesity tend to be higher, as this is generally the time when more invasive procedures (e.g. gastric bypasses) take place. If weight loss results are not sustainable, this hurts the cost efficiency of weight loss drugs and creates life-long patients which is not desirable. Therefore, more research into the long-term effects of weight loss drugs needs to be done, as the second-round effects largely determine their cost-effectiveness.
Semaglutide shortage hinders wider application
As more people are overweight globally, and weight loss drugs are an easy short-term way to lose weight, demand for weight loss drugs is strong. However, this substantial demand comes with another important drawback of weight loss drugs. Semaglutide is also the active ingredient in medicines used to treat diabetes. Due to the run on weight loss drugs, there is currently a shortage of diabetes medication worldwide.
Producers of weight loss drugs and diabetes medicine such as Novo Nordisk and Eli Lily have recently made investments to scale up production. Yet, diabetes medication is likely to stay in short supply for a while as medicine shortages are notoriously hard to solve. In light of the semaglutide shortage, it is not prudent for healthcare authorities to approve the over-the-counter sale of weight loss drugs right now. If weight loss drugs become easier to access, the shortage will likely worsen and diabetes patients might not be able to get the treatment they need.
It is a good thing that policymakers and doctors now have an additional instrument to combat the obesity epidemic. Moreover, the economic case for weight loss drugs (in Europe) is strong, especially if the long-term effects of weight loss drugs are positive.
However, as drug manufacturers like Novo Nordisk have stated: weight loss drugs are not a replacement for a healthy diet and exercise. This means that weight loss drugs are not of much use if prevention and healthier lifestyle choices are not encouraged more. Even though doctors tend to only prescribe weight loss drugs alongside a diet and exercise plan, governments need to do more. Especially because the obesity epidemic is a clear example of a market failure: the costs of a healthy lifestyle are higher than those of fast food.
To enhance collective prevention, prioritising the promotion of (moderate) exercise and increasing engagement with the food industry are essential. Governments should allocate resources towards these efforts. Interventions such as limiting the exposure of consumers to unhealthy foods, and differentiating VAT for healthy and unhealthy food could be policy options. In addition, engagement with supermarkets to stock more nutrient-dense foods could also be an avenue to pursue. Currently, it is too lucrative to promote unhealthy foods, which is something governments should act on.
For individual prevention, the use of weight loss drugs is a useful tool to get people from obesity to overweight. Yet, because of the short supply of semaglutide worldwide and the need to ensure sufficient diabetes medication, we believe it is unwise to approve weight loss drugs containing semaglutide for over-the-counter sale right now. However, we believe it should be covered in the basic health insurance for people with class 3 obesity. Weight loss drugs can make a difference for the most serious cases of obesity, and, depending on geographic location, the benefits will likely outweigh the costs.
Weight loss drugs, and Ozempic in particular, have gained significant media attention in recent years due to their use by celebrities. Elon Musk admitted using it to help him lose 30lbs, while Oprah Winfrey told People magazine last year that it was key to her dramatic weight loss. She said: “The fact that there’s a medically approved prescription for managing weight and staying healthier, in my lifetime, feels like relief, like redemption, like a gift, and not something to hide behind…”
Some users of weight loss drugs experience side effects such as nausea, stomach pain, and changes in taste which can reduce their ability to enjoy food. Therefore, it is important to only use weight loss drugs while under the supervision of a doctor and in combination with an improved diet and exercise. This is stressed by both doctors and the producers of weight loss drugs.
In short, as part of a balanced approach to fighting the obesity epidemic, weight loss drugs do have their part to play, but governments should be careful in their decision-making. The shortage of semaglutide and the accessibility of diabetes medication should be top priority. In addition, governments should encourage broad societal debates on obesity and prevention. Only then can weight loss drugs play their role in tackling the obesity epidemic.
Credit: think.ing.com
Research assesses impact of weight loss and blood sugar control in type 2 diabetes
Team Metabolic Health
A Cleveland Clinic research team has published the first study assessing the independent real-world impacts of weight loss and blood sugar control on clinical outcomes in people with type 2 diabetes treated with antidiabetic medications, and specifically with GLP-1RAs (the class of drug that includes Ozempic and Wegovy). The study found that for every 1% decrease in BMI, regardless of change in blood sugar, there was a 4% decrease in cardiovascular risk. Further, blood sugar control, independent of weight change, was linked to a lower risk of chronic kidney disease. These findings are clinically meaningful and highlight the importance of treating people with type 2 diabetes for both glycemic control and obesity.
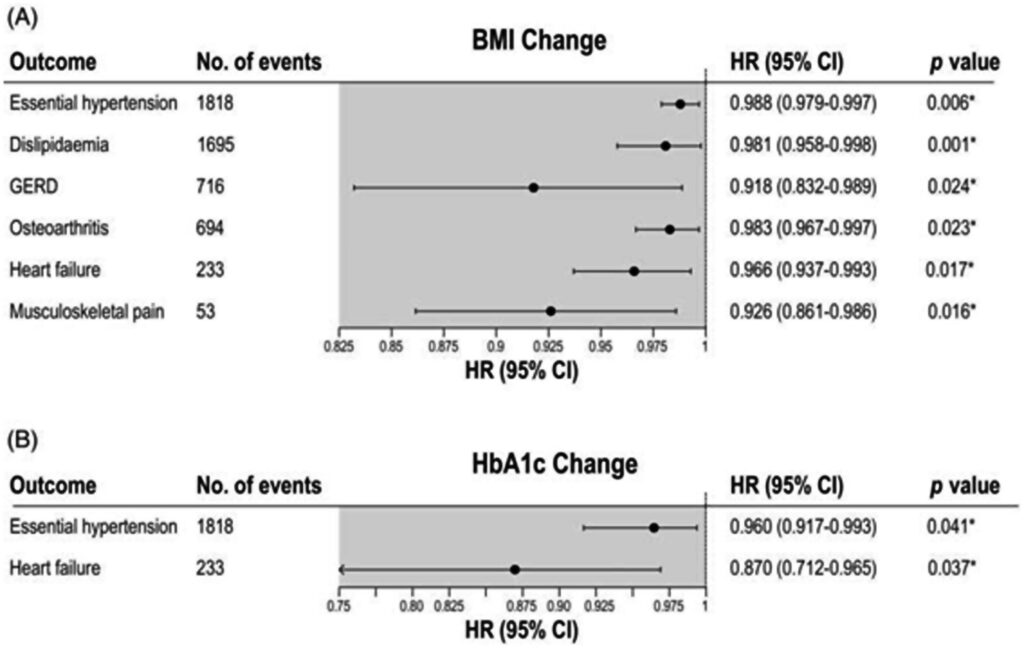
Associations of disease risk with change in body mass index (BMI) or glycated haemoglobin (HbA1c). Credit: Diabetes, Obesity and Metabolism (2024).
Credit: medicalexpress.com
While brand-name weight loss drugs are in short supply, a market for alternatives thrives
Team Metabolic Health
Prescription weight loss drugs have become so popular in the United States that suppliers have struggled to keep up. Jean Readdy, a retired teacher living in Sinking Spring, Pennsylvania, is among the one in eight Americans who have tried a GLP-1 drug for weight loss or diabetes, more commonly known by brand names like Ozempic and Wegovy.
Readdy, who has struggled with her weight for most of her life, told CBS News her weight affected her self-esteem and how she moved through the world.
“I didn’t like going out places,” Readdy admitted.
She reached her highest weight last October, right as her son was about to be married.
“I was embarrassed for him and I was embarrassed for myself,” said Readdy.
Now, she’s one of a growing number of people turning to compounded drugs: reformulated versions the FDA has permitted pharmacies to distribute during an ongoing shortage of brand-name drugs.

The big three injectable prescription weight loss medicines are Ozempic, Victoza and Wegovy.Michael Siluk/UCG/Universal Images Group via Getty Images
Readdy’s decision to switch from a name brand to a compounded drug came down to price and availability. Paying $1,200 a month for the name-brand drug Zepbound wasn’t sustainable, and it was becoming impossible to find, she said.
And she’s not alone.
Readdy turned to online communities where thousands of people shared resources and where to find the drugs in short supply. On a Reddit forum, she read about the side effects, learned about alternatives, and eventually came across a spreadsheet with dozens of telehealth providers for prescription drugs used for weight loss. After weighing the risks and calling dozens of pharmacies, she eventually found one that provided her with injectable tirzepatide, the same active ingredient found in Zepbound. Readdy now pays $399 a month for her compounded medication.
CBS News identified more than 100 companies advertising access to tirzepatide or semaglutide, both active ingredients in name-brand GLP-1 drugs that regulate insulin and suppress appetite.
LegitScript, an organization that monitors and certifies online businesses, said it saw a 94% increase in companies applying for its healthcare certification since 2023. More than half of its recent applicants had a weight-loss focus on their website.
However, compounded drugs aren’t reviewed for efficacy and safety by the FDA.
“There is not a tremendous amount of oversight,” said CBS News medical contributor Dr. Celine Gounder. “There is a wide range in terms of the quality and the risks.”
Researchers who ordered and tested compounded semaglutide found some were contaminated and others contained more of the active ingredient than advertised.
Compounded drugs typically come with a needle and a vial, rather than a pre-filled pen, as the brand-name medications do. This can make them harder to administer and lead to potential dosing errors. The FDA issued warnings about administering the proper dosage of the drugs and the risks of using compounded semaglutide.
Still, many of the telehealth companies advertising compounded weight-loss drugs present them as the same as or “generic” versions of the brand-name medications. Nearly a quarter of the websites that CBS News identified did not disclose the drugs they were advertising were compounded.
There is no FDA-approved generic version of brand-name weight loss drugs since pharmaceutical companies still hold patents on the medications. Some of the companies falsely claimed the drugs were FDA-approved. A few even allowed direct purchases without the required prescription.
The FDA is working closely with drugmakers and may restrict the manufacturing of compounded drugs as more versions of approved drugs come off the shortage list.
Last month, Eli Lilly announced it would reduce the cost of the lowest dose of its drug Zepbound to around $400 a month. It also launched its own telehealth company, LillyDirect.
Readdy, who has lost more than 50 pounds, said she intends to continue using her compounded medication.
“We’re very afraid actually that the drug is gonna be taken away,” she said. “I think it’s a miracle drug.”
Credit: cbsnews.com
These Diabetes Drugs Could Help Lower Your Risk of Dementia, Parkinson’s
Team Metabolic Health
Type 2 diabetes is associated with an increased risk of Alzheimer’s and Parkinson’s.
According to a new study, certain diabetes medications may significantly reduce this risk.
These drugs, called gliflozins or SGLT2 inhibitors, stop the kidneys from reabsorbing too much blood glucose to improve blood sugar levels.
Although the results of the study are encouraging, the authors call for more research to confirm their findings.
A team of scientists in Korea recently investigated a group of diabetes medications called gliflozins, or sodium-glucose cotransporter-2 (SGLT2) inhibitors.
They wanted to understand whether these drugs might reduce the risk of neurodegenerative conditions in people with type 2 diabetes (T2D).

A new study found that certain diabetes medications could help lower the risk of neurodegenerative diseases. FG Trade/Getty Images
Their analysis showed that compared to people taking other diabetes medications, those who took gliflozins were:
- 19% less likely to develop Alzheimer’s
- 20% less likely to develop Parkinson’s
- 31% less likely to develop vascular dementia
The study was published in the online issue of Neurology on September 18.
“The results are generally consistent even after adjusting for factors like blood pressure, glucose, cholesterol, and kidney function,” study author Minyoung Lee, MD, from Yonsei University College of Medicine in South Korea, said in a news release.
SGLT2 inhibitors lowered dementia, Parkinson’s risk by 22%
For this study, the researchers accessed data from 358,862 participants with type 2 diabetes and followed them for an average of 9.6 years.
By the study’s end, 6,837 participants had developed either dementia or Parkinson’s disease.
Overall, gliflozin use was associated with a 22% lower risk of developing either dementia or Parkinson’s.
When the researchers broke down the risk of specific neurodegenerative conditions, they found a 19% reduction in Alzheimer’s risk, a 20% reduction in Parkinson’s risk, and a 31% reduction in vascular dementia risk.
Daniel Truong, MD, a neurologist and medical director of the Truong Neuroscience Institute at MemorialCare Orange Coast Medical Center in Fountain Valley, CA, and editor-in-chief of the Journal of Clinical Parkinsonism and Related Disorders, shared his thoughts on the study findings with Healthline.
He said he was surprised “how consistent the benefits were across various subgroups of patients, including those with different comorbidities, such as cardiovascular disease or hypertension.” Truong was not involved in the study.
SGLT2 inhibitors help protect against neurodegenerative diseases
Gliflozins or SGLT2 inhibitors work by stopping the kidneys from reabsorbing as much glucose. This allows the body to remove the glucose in urine rather than re-entering the blood.
SGLT2 inhibitors are considered a second-line medication. In other words, doctors tend to prescribe them if a current diabetes medication is not working well enough.
Recently, there has been growing interest in this class of drugs and their protective effects against neurodegenerative conditions.
For instance, another Korean study published last month concluded that taking gliflozins was associated with a 35% lower riskTrusted Source of developing dementia compared with taking another common diabetes drug.
The latest study took a similar approach but also studied the impact of gliflozins on Parkinson’s disease.
In addition, the scientists compared gliflozins with a range of other diabetes medications, rather than the singular comparison drug in the previous study.
What’s the link between diabetes and neurodegenerative diseases?
Insulin primes the body’s cells to absorb blood sugar more efficiently, thereby lowering blood sugar levels.
In type 2 diabetes, however, individuals can become insulin resistant, which means that cells stop responding adequately to insulin and no longer take up glucose as efficiently.
Evidence is mounting that insulin resistance in the brain plays an important part in neurodegenerative conditions. As blood sugar levels rise, sensitive brain cells can become damaged.
A recent meta-analysisTrusted Source, for instance, found that diabetes is associated with a significantly higher risk of developing dementia.
Similarly, individuals with type 2 diabetes have a 21%Trusted Source increased risk of developing Parkinson’s disease. Evidence also suggests that the condition may progress more quickly in people with type 2 diabetes.
“An appropriate response to insulin is important not only for the pancreas and many organs in the body but also for the brain,” explained Alvaro Pascual-Leone, MD, professor of neurology at Harvard Medical School and chief medical officer and co-founder of Linus Health. Pascual-Leone was not involved in the study.
“Insulin resistance may play a key role in the link between type 2 diabetes and Alzheimer’s disease, but also other causes of dementia,” he told Healthline.
Top of Form
Enjoy a free diabetes-friendly snack list
Our printable list compiles our favorite nutritious snack ideas to help you manage your blood sugar levels. Join our diabetes newsletter for your free copy and expert guidance twice a week.
Bottom of Form
Combining metformin with gliflozins may further reduce risk
As diabetes prevalence increases, more people may face higher risks of developing neurodegenerative conditions as they grow older.
While the study authors suggest that gliflozins may just slow the progress of neurodegeneration, rather than stop it altogether, this would significantly benefit the aging population, nonetheless.
Still, the study does have some limitations. The researchers note because these neurodegenerative conditions take many years to develop, some people who did not develop dementia or Parkinson’s during the study might develop these conditions later.
“More research is needed to validate the long-term validity of these findings,” Lee said.
The study also leaves us with some unanswered questions.
For instance, the authors wonder whether starting treatment with gliflozins earlier might reduce the risk of neurodegeneration even further. This may be another reason why it’s best to start treatment as soon as possible.
Also, the researchers found that combining metformin with gliflozins reduced Parkinson’s and dementia risk to a greater extent than any other combination of drugs.
This raises the tantalizing possibility that drug combinations might be even more effective.
“To optimize antidiabetic drug use in clinical practice for neurodegenerative diseases, future research should evaluate the synergistic association of [gliflozins] with various combination therapies,” the authors wrote.
Could gliflozins reduce dementia risk in people without diabetes?
It’s currently unclear whether gliflozins could also reduce the risk of neurodegenerative conditions in people without type 2 diabetes.
“Further research needs to be done to determine if gliflozins can be neuroprotective and improve brain health and decrease dementia in people without diabetes,” explained Clifford Segil, a neurologist at Providence Saint John’s Health Center in Santa Monica, CA, who was not involved in the study.
“With their widespread use, it should be clear within a decade whether this is true. We may know the answer by 2035,” Segal added.
Truong noted these drugs do “have the potential to form the basis for future anti-dementia drugs, particularly for people at increased risk of developing dementia.”
“Their ability to improve brain metabolism, reduce inflammation, and protect cardiovascular health aligns with the primary risk factors and mechanisms driving dementia,” he continued.
“These significant effects on reducing the risk of dementia and neurodegenerative diseases represent an exciting development in diabetes care with broader implications for public health,” Truong concluded.
Top of Form
Eating well for diabetes, simplified — in just 10 mins
Our free weekly micro-lessons can empower you with wisdom you need to make healthy changes for your diabetes. Short and easy to follow tips for the week ahead.
Bottom of Form
A recent study concludes that people with type 2 diabetes who take a class of drugs called gliflozins or SGLT2 inhibitors have a significantly reduced risk of developing dementia and Parkinson’s disease.
Although further research is needed, the results add to existing evidence showing the effects of gliflozins on slowing neurodegeneration.
Credit: healthline.com
